Sonneratia alba Fruit Extract’s Potential to Reduce Atherogenic Index of Plasma and Prevent Atherogenesis in Aortic Arch of High-Fat Diet Induced Wistar Rats
Main Article Content
Abstract
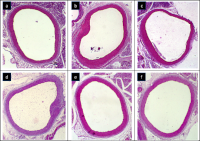
Treatments for atherosclerosis have advanced, however many still come with adverse effects and limitations. Using safe, effective, and affordable natural compounds—like those found in Sonneratia alba fruit—shows promise as a potential alternative therapy. S. alba is known for its strong antioxidant, antidiabetic, antibiotic, and anti-inflammatory properties. This study aims to explore how S. alba fruit extract affects atherosclerosis risk and atherogenesis in high-fat diet (HFD) induced rats. This study used 24 male Wistar rats, aged 8–10 weeks and weighing 170–190 g, divided into six groups: a normal group, a positive control group receiving HFD, a group receiving HFD plus atorvastatin (10 mg/day), and three groups receiving HFD and S. alba extract at doses of 200, 400, and 800 mg/kg/day. The HFD was given 20 g/day for 10 weeks, while atorvastatin and S. alba extract were administered orally throughout the same period. Lipid profiles, LDL/HDL ratio and atherogenic index of plasma (AIP) were measured at weeks 5 and 10. The aortic arches were collected, processed into histological hematoxylin-eosin slides. Alterations of aortic structure were examined under a microscope and scored. The results showed S. alba extract has strong antioxidant properties. Giving S. alba at a dose of 800 mg/kg/day significantly reduced LDL/HDL ratio and AIP at both weeks 5 and 10. Histopathological analysis supported these findings, showing that S. alba extract significantly inhibited atherogenesis at the same dose. In conclusion, S. alba fruit extract may lower atherosclerosis risk and prevent atherogenesis in aorta of HFD-induced rats.
Downloads
Article Details
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
How to Cite
References
1. Ralapanawa U, Sivakanesan R. Epidemiology and the magnitude of coronary artery disease and acute coronary syndrome: A narrative review. J Epidemiol Glob Health. 2021; 11(2):169. doi:10.2991/jegh.k.201217.001
2. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V. Global burden of cardiovascular diseases and risk factors, 1990–2019. J Am Coll Cardiol. 2020; 76(25):2982-3021. doi:10.1016/j.jacc.2020.11.010
3. Mehu M, Narasimhulu CA, Singla DK. Inflammatory cells in atherosclerosis. Antioxidants. 2022; 11(2):233. doi:10.3390/antiox11020233
4. Libby P, Buring JE, Badimon L, Hansson GK, Deanfield J, Bittencourt MS, Tokgozoglu L, Lewis EF. Atherosclerosis. Nat Rev Dis Prim. 2019; 5(1):56. doi:10.1038/s41572-019-0106-z
5. Chen M, Fang CY, Guo JC, Pang LM, Zhou Y, Hong Y, Yang LF, Zhang J, Zhang T, Zhou BF, Hu GQ. Predictive value of atherogenic index of plasma and atherogenic index of plasma combined with low-density lipoprotein cholesterol for the risk of acute myocardial infarction. Front Cardiovasc Med. 2023; 10:1117362. doi:10.3389/fcvm.2023.1117362
6. Khatiwada N, Hong Z. Potential benefits and risks associated with the use of statins. Pharmaceutics. 2024; 16(2). doi:10.3390/pharmaceutics16020214
7. Zhong C, Deng K, Lang X, Shan D, Xie Y, Pan W, Yu J. Therapeutic potential of natural flavonoids in atherosclerosis through endothelium-protective mechanisms: An update. Pharmacol Ther. 2025; 271:108864. doi:10.1016/j.pharmthera.2025.108864
8. Kulkarnii CP, Manohar SM. A review of botany, phytochemistry, and pharmacology of the mangrove apple Sonneratia alba J. Sm. J Appl Pharm Sci. 2024; 14(5). doi:10.7324/JAPS.2024.181289
9. Parthiban A, Sivasankar R, Sachithanandam V, Khan SA, Jayshree A, Murugan K, Sridhar R. An integrative review on bioactive compounds from Indian mangroves for future drug discovery. South African J Bot. 2022; 149:899-915. doi:10.1016/j.sajb.2021.10.004
10. Sachithanandam V, Lalitha P, Parthiban A, Mageswaran T, Manmadhan K, Sridhar R. A review on antidiabetic properties of indian mangrove plants with reference to island ecosystem. Evid Based Complement Alternat Med. 2019; 2019:4305148. doi:10.1155/2019/4305148
11. Muhaimin M, Latifah N, Chaerunisaa AY, Subarnas A, Susilawati Y, Hirzan R. Antiplasmodial activity of ethanol extract of Sonneratia alba leaves. Trop J Nat Prod Res. 2024; 8(4):6884-6890. doi:10.26538/tjnpr/v8i4.19
12. Morada N, Metillo E, Uy M, Oclarit J. Anti diabetic polysaccharide from mangrove plant, Sonneratia alba Sm. Int Proc Chem Biol Env Eng. 2011; 3:197-200
13. J.A Musa W, Bialangi N, Situmeang B, Silaban S. Triterpenoid compound from metanol extract of mangrove leaves (Sonneratia alba) and anti-cholesterol activity test. J Pendidik Kim. 2019; 11(1):18-23. doi:10.24114/jpkim.v11i1.13124
14. Morada NJ, Metillo EB, Uy MM, Oclarit JM. Toxicity and hypoglycemic effect of tannin-containing extract from the mangrove tree Sonneratia alba Sm. Bull Environ Pharmacol Life Sci. 2016; 5(6):58-64.
15. Masdar H, Hamidy MY, Darmawi, Trihardi R, Perwira A, Utari D. Anti-atherosclerotic effects of Sonneratia alba fruit extract in atherosclerotic-induced rats. Int J Appl Pharm. 2020:41-43. doi:10.22159/ijap.2020.v12s3.39467
16. Khwunsiriwong, Sichaem, Jaramornburapong, Premjit, Funnimid, Niyomdecha. Phytochemical screening, total flavonoid and phenolic contents, and antioxidant activities of thai mango (Mangifera indica L.) extracts. Trop J Nat Prod Res. 2025; 6(9). doi:10.26538/tjnpr/v9i6.17
17. Cahyadi J, Satriani GI, Gusman E, Weliyadi E. Inhibiting Vibrio harveyi infection in Penaeus monodon using enriched Artemia salina with mangrove fruit Sonneratia alba extract. AACL Bioflux. 2020; 13(3):1674-1681. Accessed September 15, 2025. https://bioflux.com.ro/docs/2020.1674-1681.pdf
18. Siahaya VG, Moniharapon T, Mailoa MN, Leatemia JA. Potential of mangrove apples (Sonneratia alba) as a botanical insecticide. Mod Appl Sci. 2017; 12(1):1. doi:10.5539/mas.v12n1p1
19. Ragasa CY, Ebajo VD, De Los Reyes MM, Mandia EH, Brkljača R, Urban S. Triterpenes and sterols from Sonneratia alba. Int J Curr Pharm Rev Res. 2015; 6(6):256-261. Accessed July 8, 2025. https://impactfactor.org/PDF/IJCPR/6/IJCPR,Vol6,Issue6,Article3.pdf
20. Rozirwan, Nugroho RY, Hendri M, Fauziyah, Putri WAE, Agussalim A. Phytochemical profile and toxicity of extracts from the leaf of Avicennia marina (Forssk.) Vierh. collected in mangrove areas affected by port activities. South African J Bot. 2022; 150:903-919. doi:10.1016/j.sajb.2022.08.037
21. Deviarni IM, Yunus A, Prabawa S, Anam C. Antioxidant activity and bioactive compound identification in Sonneratia alba fruit. IOP Conf Ser Earth Environ Sci. 2025; 1490(1):012029. doi:10.1088/1755-1315/1490/1/012029
22. Paputungan Z, Wonggo D, Kaseger BE. Phytochemical and antioxidant activity anylisis of Sonneratia alba fruit in Nunuk Village, Pinolosian District, South Bolaang Mongondow, North Sulawesi. Media Teknol Has Perikan. 2017; 5(3):96. doi:10.35800/mthp.5.3.2017.16866
23. Michiels JA, Kevers C, Pincemail J, Defraigne JO, Dommes J. Extraction conditions can greatly influence antioxidant capacity assays in plant food matrices. Food Chem. 2012; 130(4):986-993. doi:10.1016/j.foodchem.2011.07.117
24. Jariyah, Azkiyah L, Wijanarko SB, Estiasih T, Yuwono SS, Yunianta. Hypocholesterolemic effect of pedada (Sonneratia caseolaris) fruit flour in Wistar rat. Int J PharmTech Reseacrh. 2013; 5(4):1619-1627..
25. Amalia R, Pramono A, Afifah DN, Noer ER, Muniroh M, Kumoro AC. Mangrove fruit (Bruguiera gymnorhiza) increases circulating GLP-1 and PYY, modulates lipid profiles, and reduces systemic inflammation by improving SCFA levels in obese Wistar rats. Heliyon. 2022; 8(10):e10887. doi:10.1016/j.heliyon.2022.e10887
26. De Souza Mesquita LM, Caria CREP, Santos PS, Ruy CC, Da Silma Lima N, Moreira DKT, Da Rocha CQ, Murador DC, De Rosso VV, Gambero A, Vilegas W. Modulatory effect of polyphenolic compounds from the mangrove tree Rhizophora
mangle L. on non-alcoholic fatty liver disease and insulin resistance in high-fat diet obese mice. Molecules. 2018; 23(9). doi:10.3390/molecules23092114
27. Toma L, Sanda G, Niculescu L, Deleanu M, Sima A, Stancu C. Phenolic compounds exerting lipid-regulatory, anti-inflammatory and epigenetic effects as complementary treatments in cardiovascular diseases. Biomolecules. 2020;10(4):641. doi:10.3390/biom10040641
28. Hamer M, O’Donovan G, Stamatakis E. High-density lipoprotein cholesterol and mortality. Arterioscler Thromb Vasc Biol. 2018; 38(3):669-672. doi:10.1161/ATVBAHA.117.310587
29. Shin S, Ha T, McGregor RA, Choi M. Long‐term curcumin administration protects against atherosclerosis via hepatic regulation of lipoprotein cholesterol metabolism. Mol Nutr Food Res. 2011; 55(12):1829-1840. doi:10.1002/mnfr.201100440
30. Mollazadeh H, Mahdian D, Hosseinzadeh H. Medicinal plants in treatment of hypertriglyceridemia: A review based on their mechanisms and effectiveness. Phytomedicine. 2019;53:43-52. doi:10.1016/j.phymed.2018.09.024
31. Sun T, Chen M, Shen H, Pingyin, Fan L, Chen X, Wu J, Xu Z, Zhang J. Predictive value of LDL/HDL ratio in coronary atherosclerotic heart disease. BMC Cardiovasc Disord. 2022; 22(1):273. doi:10.1186/s12872-022-02706-6
32. Assempoor R, Daneshvar MS, Taghvaei A, Abroy AS, Azimi A, Nelson JR, Hosseini K. Atherogenic index of plasma and coronary artery disease: a systematic review and meta-analysis of observational studies. Cardiovasc Diabetol. 2025; 24(1):35. doi:10.1186/s12933-025-02582-2
33. Millán J, Pintó X, Muñoz A, Zuniga M, Rubies-Prat J, Pallardo LF, Masana L, Mangas A, Hernadez-Mijares A, Gonzales-Santos P, Ascaso JF, Pedro-Botet J. Lipoprotein ratios: Physiological significance and clinical usefulness in cardiovascular prevention. Vasc Health Risk Manag. 2009;5:757-765.
34. Khatana C, Saini NK, Chakrabarti S, Saini V, Sharma A, Saini RV, Adesh KS. Mechanistic insights into the oxidized low-density lipoprotein-induced atherosclerosis. Oxid Med Cell Longev. 2020; 2020:5245308. doi:10.1155/2020/5245308
35. He Y, Liu T. Oxidized low-density lipoprotein regulates macrophage polarization in atherosclerosis. Int Immunopharmacol. 2023; 120:110338. doi:10.1016/j.intimp.2023.110338
36. Förstermann U, Xia N, Li H. Roles of vascular oxidative stress and nitric oxide in the pathogenesis of atherosclerosis. Circ Res. 2017; 120(4):713-735. doi:10.1161/CIRCRESAHA.116.309326
37. Sutton G, Pugh D, Dhaun N. Developments in the role of endothelin-1 in atherosclerosis: A potential therapeutic target? Am J Hypertens. 2019; 32(9):813-815. doi:10.1093/ajh/hpz091
38. Li H, Förstermann U, Xia N, Kuntic M, Münzel T, Daiber A. Pharmacological targeting of endothelial nitric oxide synthase dysfunction and nitric oxide replacement therapy. Free Radic Biol Med. 2025; 237:455-472. doi:10.1016/j.freeradbiomed.2025.06.009
39. Liang X, Hou X, Yang Y, Liu H, Guo R, Yang Z, Yang L. The feedback loop of ‘EMMPRIN/NF-κB’ worsens atherosclerotic plaque via suppressing autophagy in macrophage. J Mol Cell Cardiol. 2018; 114:129-140. doi:10.1016/j.yjmcc.2017.11.008
40. Ochoa CD, Wu RF, Terada LS. ROS signaling and ER stress in cardiovascular disease. Mol Aspects Med. 2018;63:18-29. doi:10.1016/j.mam.2018.03.002
41. Xiang P, Blanchard V, Francis GA. Smooth muscle cell—macrophage interactions leading to foam cell formation in atherosclerosis: location, location, location. Front Physiol. 2022; 13. doi:10.3389/fphys.2022.921597
42. Akhmedov A, Sawamura T, Chen CH, Kraler S, Vdovenko D, Lüscher TF. Lectin-like oxidized low-density lipoprotein receptor-1 (LOX-1): A crucial driver of atherosclerotic cardiovascular disease. Eur Heart J. 2021; 42(18):1797-1807. doi:10.1093/eurheartj/ehaa770
43. Bennett MR, Sinha S, Owens GK. Vascular smooth muscle cells in atherosclerosis. Circ Res. 2016; 118(4):692-702. doi:10.1161/CIRCRESAHA.115.306361
44. Wu MY, Li CJ, Hou MF, Chu PY. New insights into the role of inflammation in the pathogenesis of atherosclerosis. Int J Mol Sci. 2017; 18(10):2034. doi:10.3390/ijms18102034
45. Ahmadi A, Jamialahmadi T, Sahebkar A. Polyphenols and atherosclerosis: A critical review of clinical effects on LDL oxidation. Pharmacol Res. 2022; 184:106414. doi:10.1016/j.phrs.2022.106414