Therapeutic Potential of Lactobacillus plantarum DS1 in Modulating Hypertension, Blood Sugar and Inflammation via ACE-2 Expression in Diabetic Rats
Main Article Content
Abstract
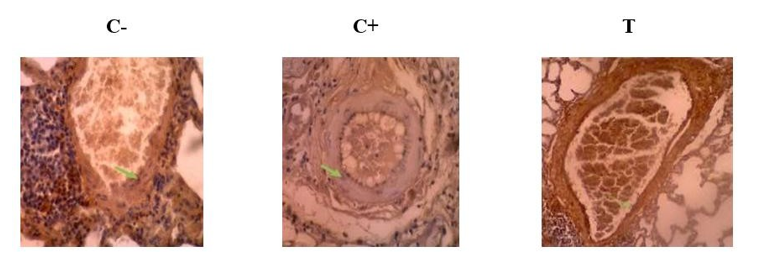
Hypertension and diabetes, two interrelated non-communicable diseases, contribute significantly to global morbidity and mortality and often trigger gut microbiota dysbiosis. Gut microbiota-based therapies, particularly probiotics, may serve as an alternative approach to managing hypertension and diabetes. This study aims to explore the therapeutic potential of Lactobacillus plantarum DS1 in modulating hypertension and inflammation by examining its effects on ACE-2 expression, providing a basis for developing probiotic therapy in chronic metabolic disorders. This study used male Wistar rats (Rattus norvegicus), which were maintained for 8 weeks. The Rattus norvegicus rats were split into three groups: group one (C-) was not treated with Lactobacillus plantarum DS1, group (C+) received a high blood sugar but was not given Lactobacillus plantarum DS1, and a treatment group (T) that received 1 mL of Lactobacillus plantarum DS1 every day per oral. Lactobacillus plantarum DS1 significantly reduced random blood sugar levels in the T group (from 241.17 mg/dl to 150.71 mg/dl). The T group showed stable systolic blood pressure (139.83 to 140.17 mmHg) and a slight decrease in diastolic blood pressure (80.33 to 78.50 mmHg), indicating that the treatment may help protect against high blood pressure. Treatment with Lactobacillus plantarum DS1 successfully lowered high ACE-2 levels in the T group, showing that it helps prevent this increase. Therefore, it is concluded that Lactobacillus plantarum DS1 effectively maintains blood pressure, lowers blood sugar, and controls inflammation in diabetic rats. Lactobacillus plantarum DS1 holds significant promise as a therapeutic agent for hypertension and inflammation in individuals with diabetes.
Downloads
Article Details
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
How to Cite
References
1. Shanmugam K J, P C, P C. Estimates of Diabetes Mellitus and Hypertension and Associated Risk Factors. Int J Health Sci Res. 2024;14(6):72–79. DOI: https://doi.org/10.52403/ijhsr.20240611
2. Mendis S, O’Brien E, Seedat YK, Yusuf S. Hypertension and Diabetes: Entry Points for Prevention and Control of the Global Cardiovascular Epidemic. Int. J. Hypertens. 2013; 2013:1–3. DOI: https://doi.org/10.1155/2013/878460
3. Da Y, Khan B, Vathsala A. The Dual Disease Burden of Hypertension and Diabetes. S Ram CV, editor. Johtn. 2018;4(2):100–106. DOI: https://doi.org/10.15713/ins.johtn.0113
4. Rajalakshmi R, Prathiba V, Raman R, Ruamviboonsuk P, Pradeepa R, Mohan V. The Burden of Non-communicable Diseases and Diabetic Retinopathy. In: Das T, Nayar PD, editors. South-East Asia Eye Health [Internet]. Singapore: Springer Singapore; 2021 [cited 2025 June 6]. p. 197–228. Available from: https://link.springer.com/10.1007/978-981-16-3787-2_12 DOI: https://doi.org/10.1007/978-981-16-3787-2_12
5. Rodriguez-Iturbe B, Pons H, Johnson RJ. Role of the Immune System in Hypertension. Physiol. Rev. 2017;97(3):1127–1164. DOI: https://doi.org/10.1152/physrev.00031.2016
6. Lastra G, Syed S, Kurukulasuriya LR, Manrique C, Sowers JR. Type 2 Diabetes Mellitus and Hypertension. Endocrinol. Metab. Clin. North Am. 2014;43(1):103–122. DOI: https://doi.org/10.1016/j.ecl.2013.09.005
7. Rizvi S, Khan F, Fatima N, Raza ST, Rashid G, Mahdi F. Probiotics in Diabetes Mellitus. In: Probiotics [Internet]. 1st ed. Boca Raton: CRC Press; 2024 [cited 2025 June 6]. p. 159–87. Available from: https://www.taylorfrancis.com/books/9781003452249/chapters/10.1201/9781003452249-8 DOI: https://doi.org/10.1201/9781003452249-8
8. Nugraha IS, Suastini NM, Santi MDS. Role of Probiotics in Type 2 Diabetes Mellitus Patients with Hypertension: A REVIEW. JPSA. 2023;5(2):70-76. DOI: https://doi.org/10.24843/JPSA.2023.v05.i02.p03
9. Sreepathi N, Jayanthi MK, Chandra SJ, Bajpe SN, Ramu R. Probiotic Intervention in the Treatment of Diabetes Mellitus: A Review. J Pure Appl Microbiol. 2022;16(3):1519–1529. DOI: https://doi.org/10.22207/JPAM.16.3.25
10. Ayesha IE, Monson NR, Klair N, Patel U, Saxena A, Patel D, Venugopal S, Ayesha IE. Probiotics and their role in the management of type 2 diabetes mellitus (Short-term versus long-term effect): A systematic review and meta-analysis. Cureus. 2023;15(10). DOI: https://doi.org/10.7759/cureus.46741
11. Sun Z, Dong C. The Application and Research of Probiotics in the Treatment of Diabetes. WJIMT. 2024;7(5):145–150. DOI: https://doi.org/10.53469/wjimt.2024.07(05).18
12. Zikou E, Dovrolis N, Dimosthenopoulos C, Gazouli M, Makrilakis K. The Effect of Probiotic Supplements on Metabolic Parameters of People with Type 2 Diabetes in Greece—A Randomized, Double-Blind, Placebo-Controlled Study. Nutrients. 2023;15(21):4663. DOI: https://doi.org/10.3390/nu15214663
13. Okediya CK, Oyewale JO, Okediya TT, Ajayi AS, Olasehinde G Effect of Lactobacillus acidophilus and Lactobacillus plantarum on Weight Reduction in Obese Rats. TJNPR. 20213;5(4):759–762. DOI: https://doi.org/10.26538/tjnpr/v5i4.27
14. AkbariRad M, Shariatmaghani SS, Razavi BM, Majd HM, Shakhsemampour Z, Sarabi M, Esfandiari S, Azadbakht M, Karimi G. Probiotics for glycemic and lipid profile control of the pre-diabetic patients: a randomized, double-blinded, placebo-controlled clinical trial study. Diabetol Metab Syndr. 2023; 15(1): 41. DOI: https://doi.org/10.1186/s13098-023-01050-9
15. Wang Y, Xie D, Zhao L, Chen Z, Zhang Y, Du L, Wang L, Sun Y, Hu X, Zhou W. Antihypertensive and gut microbiota regulatory effects of yeast protein hydrolysate on spontaneous hypertensive rats. Process Biochem. 2024; 140: 66–77. DOI: https://doi.org/10.1016/j.procbio.2024.02.008
16. Hardjo Lugito NP, Djuwita R, Adisasmita A, Simadibrata M. Blood pressure lowering effect of Lactobacillus-containing probiotic. Int J Pharm Pharmacol. 2022; 17(1): 1–13. DOI: https://doi.org/10.37290/ijpp2641-7197.17:1-13
17. Song H, Xue H, Zhang Z, Wang J, Li A, Zhang J, Yang Y, Zhao H, Zhang H. Amelioration of type 2 diabetes using four strains of Lactobacillus probiotics: effects on gut microbiota reconstitution-mediated regulation of glucose homeostasis, inflammation, and oxidative stress in mice. J Agric Food Chem. 2023; 71(51): 20801–20814. DOI: https://doi.org/10.1021/acs.jafc.3c04665
18. Wang Z, Wu J, Tian Z, Si Y, Chen H, Gan J. The mechanisms of the potential probiotic Lactiplantibacillus plantarum against cardiovascular disease and the recent developments in its fermented foods. Foods. 2022; 11(17): 2549. DOI: https://doi.org/10.3390/foods11172549
19. Jiménez Soto RE, Vanegas Espinoza JI, Cárdenas Chacha KG, Macas González LA, Jima Blacio JJ. Implicaciones de Lactobacillus plantarum en trastornos patológicos: Revisión bibliográfica. Cienc Lat. 2024; 8(4): 4959–4978. DOI: https://doi.org/10.37811/cl_rcm.v8i4.12721
20. Toshimitsu T, Gotou A, Sashihara T, Hojo K, Hachimura S, Shioya N, Suzuki T, Kaneko K, Suganuma H, Ishida Y, Koga Y. Ingesting probiotic yogurt containing Lactiplantibacillus plantarum OLL2712 improves glycaemic control in adults with prediabetes in a randomized, double-blind, placebo-controlled trial. Diabetes Obes Metab. 2024; 26(6): 2239–2247. DOI: https://doi.org/10.1111/dom.15534
21. 21. Daliri EBM, Lee BH, Oh DH. Current perspectives on antihypertensive probiotics. Probiotics Antimicro Prot. 2017; 9(2): 91–101. DOI: https://doi.org/10.1007/s12602-016-9241-y
22. Ma Y, Fei Y, Han X, Liu G, Fang J. Lactobacillus plantarum alleviates obesity by altering the composition of the gut microbiota in high-fat diet-fed mice. Front Nutr. 2022; 9: 947367.
23. Hao X, Xia Y, Wang Y, Zhang X, Liu L. The addition of probiotics promotes the release of ACE-I peptide of Cheddar cheese: Peptide profile and molecular docking. Int Dairy J. 2023; 137: 105507. DOI: https://doi.org/10.1016/j.idairyj.2022.105507
24. Lescheid DW. Probiotics as regulators of inflammation: A review. Funct Foods Health Dis. 2014; 4(7): 299–311. DOI: https://doi.org/10.31989/ffhd.v4i7.2
25. Divyashri G, Krishna G, Muralidhara, Prapulla SG. Probiotic attributes, antioxidant, anti-inflammatory, and neuromodulatory effects of Enterococcus faecium CFR 3003: in vitro and in vivo evidence. J Med Microbiol. 2015; 64(12): 1527–1540. DOI: https://doi.org/10.1099/jmm.0.000184
26. Carter CS, Morgan D, Verma A, Lobaton G, Aquino V, Sumners E, Raizada MK, Gao L, Buford TW, Carter JD, Fadel PJ, Chappell MC, Ericson ME, Liu X, Herold KC, Musi N, Ahmad S, Katovich MJ. Therapeutic delivery of Ang(1–7) via genetically modified probiotic: A dosing study. J Gerontol A Biol Sci Med Sci. 2020; 75(7): 1299–1303. DOI: https://doi.org/10.1093/gerona/glz222
27. Lee YS, Lee D, Park GS, Ko SH, Park J, Lee YK, Lee HJ, Kim J, Lee S. Lactobacillus plantarum HAC01 ameliorates type 2 diabetes in high-fat diet and streptozotocin-induced diabetic mice in association with modulating the gut microbiota. Food Funct. 2021; 12(14): 6363–6373. DOI: https://doi.org/10.1039/D1FO00698C
28. Yorek M. Treatment for diabetic peripheral neuropathy: What have we learned from animal models? Curr Diab Rep. 2022; 18(5): e040521193121. DOI: https://doi.org/10.2174/1573399817666210504101609
29. Wolfensohn S, Lloyd M. Handbook of laboratory animal management and welfare. 4th ed. Chichester, West Sussex, UK: Wiley-Blackwell; 2013. p. 371–378.
30. Sharifi-Rad J, Rodrigues CF, Stojanović-Radić Z, Dimitrijević M, Aleksić A, Neffe-Skocińska K, Zielińska D, Kołożyn-Krajewska D, Salehi B, Prabu SM, Taheri Y, Suleria HAR. Probiotics: Versatile bioactive components in promoting human health. Medicina. 2020; 56(9): 433. DOI: https://doi.org/10.3390/medicina56090433
31. Jacouton E, Mondot S, Langella P, Bermúdez-Humarán LG. Impact of oral administration of Lactiplantibacillus plantarum strain CNCM I−4459 on obesity induced by high-fat diet in mice. Bioeng. 2023; 10(10): 1151.
32. Montachana Crespata MA, Viteri Robayo CP. Effect of probiotics on the obese patient: A review study. Salud Cienc Tecnol. 2023; 3: 883. DOI: https://doi.org/10.56294/saludcyt2023883
33. Yadav H, Lee JH, Lloyd J, Walter P, Rane SG. Beneficial metabolic effects of a probiotic via butyrate-induced GLP-1 hormone secretion. J Biol Chem. 2013; 288(35): 25088–25097. DOI: https://doi.org/10.1074/jbc.M113.452516
34. Park DY, Ahn YT, Park SH, Huh CS, Yoo SR, Yu R, Sung MK, McGregor RA, Choi MS. Supplementation of Lactobacillus curvatus HY7601 and Lactobacillus plantarum KY1032 in diet-induced obese mice is associated with gut microbial changes and reduction in obesity. PLoS ONE. 2013; 8(3): e59470. DOI: https://doi.org/10.1371/journal.pone.0059470
35. Jacouton E, Mondot S, Langella P, Bermúdez-Humarán LG. Impact of oral administration of Lactiplantibacillus plantarum strain CNCM I−4459 on obesity induced by high-fat diet in mice. Bioeng. 2023; 10: 1151. DOI: https://doi.org/10.3390/bioengineering10101151
36. Kim KH, Hwang Y, Kang SS. Regulatory effect of spray-dried Lactiplantibacillus plantarum K79 on the activation of vasodilatory factors and inflammatory responses. Food Sci Anim Resour. 2024; 44(1): 216–224. DOI: https://doi.org/10.5851/kosfa.2023.e78
37. Khalesi S, Sun J, Buys N, Jayasinghe R. Effect of probiotics on blood pressure: A systematic review and meta-analysis of randomized, controlled trials. Hypertension. 2014; 64(4): 897–903. DOI: https://doi.org/10.1161/HYPERTENSIONAHA.114.03469
38. Zhong H, Wang L, Jia F, Yan Y, Xiong F, Li Y, Yu J, Wei H, Zhang W, Zhu J. Effects of Lactobacillus plantarum supplementation on glucose and lipid metabolism in type 2 diabetes mellitus and prediabetes: A systematic review and meta-analysis of randomized controlled trials. Clin Nutr ESPEN. 2024; 61: 377–384. DOI: https://doi.org/10.1016/j.clnesp.2024.04.009
39. Ma Y, Fei Y, Han X, Liu G, Fang J. Lactobacillus plantarum alleviates obesity by altering the composition of the gut microbiota in high-fat diet-fed mice. Front Nutr. 2022; 9: 947367. DOI: https://doi.org/10.3389/fnut.2022.947367
40. Kim JH, Kwak W, Nam Y, Baek J, Lee Y, Yoon S, Park T, Choi Y, Kim S, Lee H. Effect of postbiotic Lactiplantibacillus plantarum LRCC5314 supplemented in powdered milk on type 2 diabetes in mice. J Dairy Sci. 2024; 107(8): 5301–5315. DOI: https://doi.org/10.3168/jds.2023-24103
41. Qi D, Nie XL, Zhang JJ. Retracted article: The effect of probiotics supplementation on blood pressure: A systemic review and meta-analysis. Lipids Health Dis. 2020; 19(1): 79. DOI: https://doi.org/10.1186/s12944-020-01259-x
42. Das S, Hati S. Food-derived ACE inhibitory peptides. In: Nutrition and functional foods in boosting digestion, metabolism and immune health. Elsevier; 2022. p. 39–54. DOI: https://doi.org/10.1016/B978-0-12-821232-5.00006-9
43. Investigation of angiotensin-converting enzyme inhibitory effects of Indonesian traditional medicine (Jamu). Trop J Nat Prod Res. 2021; 5(4): 692–697. DOI: https://doi.org/10.26538/tjnpr/v5i4.17
44. Wikandari PR, Herdyastuti N, Tukiran, Wati FA, Dzulkarnain SA. The potential of single bulb garlic fermented with Lactobacillus plantarum B1765 to manage gluconeogenesis and inflammation in type-2 diabetes mellitus rats. Trop J Nat Prod Res. 2025; 9(??): 2002–2006. DOI: https://doi.org/10.26538/tjnpr/v9i5.18
45. Yu J, Sun M, Jiang S, Jiang C, Mu G, Tuo Y. Oral administration of fermented milk from co-starter containing Lactobacillus plantarum Y44 shows an ameliorating effect on hypertension in spontaneously hypertensive rats. Foods. 2024; 13(5): 641. DOI: https://doi.org/10.3390/foods13050641
46. De Assis Gadelha DD, De Brito Alves JL, Da Costa PCT, Da Luz MS, De Oliveira Cavalcanti C, Bezerril FF, Fernandes VO, De Oliveira Junior FM, Leandro CG, De Andrade RV, De Oliveira JC, De Almeida RN. Lactobacillus group and arterial hypertension: A broad review on effects and proposed mechanisms. Crit Rev Food Sci Nutr. 2024; 64(12): 3839–3860. DOI: https://doi.org/10.1080/10408398.2022.2136618
47. Robles-Vera I, Toral M, Romero M, Jiménez R, Sánchez M, Pérez-Vizcaíno F, Duarte J. Antihypertensive Effects of Probiotics. Curr Hypertens Rep. 2017; 19(4):26. DOI: https://doi.org/10.1007/s11906-017-0723-4
48. Yuan L, Li Y, Chen M, Xue L, Wang J, Ding Y, Zhang H, Liu C, Zhao J, Zhang H. Antihypertensive activity of milk fermented by Lactiplantibacillus plantarum SR37-3 and SR61-2 in L-NAME-induced hypertensive rats. Foods. 2022; 11(15):2332 DOI: https://doi.org/10.3390/foods11152332