Structure-Based Discovery of Immunomodulators for Stunting Inspired by Caulerpin: A Rational Approach Targeting Immune Homeostasis
Main Article Content
Abstract
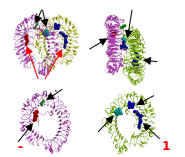
Stunting remains a critical public health issue, affecting millions globally and hundreds of thousands in Indonesia annually, thus demanding innovative interventions. While immune dysfunction is implicated in the pathogenesis of stunting, it is often underemphasized in
therapeutic strategies. This study leverages structure-based drug design and similarity searching to identify novel immunomodulators with potential application in stunting
treatment. Initial molecular docking revealed that caulerpin (1), an algal alkaloid, exhibited promising binding to immune-related targets. However, its suboptimal drug-likeness
prompted the use of SwissSimilarity structural search, leading to the identification of CPG-
52852 (7), a TLR7 agonist. Compound 7 demonstrated strong predicted immunomodulatory
properties via PASS analysis. Further similarity searching, using 7 as a query, identified imiquimod (8) and resiquimod (9), sharing similar imidazoquinolinone scaffold with 7.
Building upon the scaffold, de novo design of R848 with Metatox generated ten novel
compounds (12-21) with predicted immunomodulatory activity nearly equal or improved drug-likeness with ADMET score of 0.25, 0.28, 0.28, and 0.32 for compounds 13, 14, 15, and 17 compared to 0.29 for their parent molecule, R848. Unlike the TLR-7/8 agonist R848, compounds 13, 14, 15, and 17 preferentially interacted with amino acid residues unrelated to the ones reported for the TLR-7/8 agonist, suggesting a distinct mechanism of action (e.g., antagonism or allosteric modulation). These allosteric modulators represent promising leads for treating immune dysfunction-related diseases, including stunting, where alternative mechanisms beyond direct agonism are needed.
Downloads
Article Details
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
How to Cite
References
Khani Jeihooni A, Mohammadkhah F, Razmjouie F, Harsini PA, Sedghi Jahromi F. Effect of Educational Intervention Based on Health Belief Model on Mothers Monitoring Growth of 6–12 Months Child with Growth Disorders. BMC Pediatr. 2022; 22(1):1–11. DOI: https://doi.org/10.1186/s12887-022-03593-8
Tzioumis E, Kay MC, Bentley ME, Adair LS. Prevalence and Trends in the Childhood Dual Burden of Malnutrition in Low- and Middle-Income Countries, 1990-2012. Public Health Nutr. 2016; 19(8):1375–1388. DOI: https://doi.org/10.1017/S1368980016000276
Surono IS, Jalal F, Bahri S, Romulo A, Kusumo PD, Manalu E, Yusnita, Venema K. Differences in Immune Status and Fecal SCFA Between Indonesian Stunted Children and Children with Normal Nutritional Status. PLoS One. 2021; 16(7):1–14. DOI: https://doi.org/10.1371/journal.pone.0254300
Quamme SH and Iversen PO. Prevalence of Child Stunting in Sub-Saharan Africa and Its Risk Factors. Clin Nutr Open Sci. 2022; 42:49–61. DOI: https://doi.org/10.1016/j.nutos.2022.01.009
World Health Organization. WHO. Global Nutrition Targets 2025: Stunting Policy Brief. 2014. Available from: https://www.who.int/publications/i/item/WHO-NMH-NHD-14.3
UNICEF, WHO, World Bank Group. Levels and Trends in Child Malnutrition: UNICEF/WHO/The World Bank Group Joint Child Malnutrition Estimates: Key Findings of the 2021 Edition. 2021. Available from: https://www.who.int/publications/i/item/9789240025257
de Onis M and Branca F. Childhood Stunting: A Global Perspective. Matern Child Nutr. 2016; 12:12–26. DOI: https://doi.org/10.1111/mcn.12231
Bourke CD, Berkley JA, Prendergast AJ. Immune Dysfunction as a Cause and Consequence of Malnutrition. Trends Immunol. 2016; 37(6):386–398. DOI: https://doi.org/10.1016/j.it.2016.04.003
Gharpure R, Mor SM, Viney M, Hodobo T, Lello J, Siwila J, Dube K, Robertson R, Mutasa K, Berger C, Hirai M, Brown T, Ntozini R, Evans C, Hoto P, Smith L, Tavengwa N, Joyeux M, Humphrey J, Berendes D, Prendergast A. A One Health Approach to Child Stunting: Evidence and Research Agenda. Am J Trop Med Hyg. 2021; 104(5):1620–1624. DOI: https://doi.org/10.4269/ajtmh.20-1129
Firmansyah RRT, Murti B, Prasetya H. A Meta-Analysis of Correlation Between Diarrhea and Stunting in Children Under Five. J Epidemiol Public Health. 2023; 8(1):88–97. DOI: https://doi.org/10.26911/jepublichealth.2023.08.01.08
Kraemer K. The Stunting Enigma. Sight Life. 2013; 27(2):12–16. DOI: https://doi.org/10.52439/XWLM4869
Smith LE, Stoltzfus RJ, Prendergast A. Food Chain Mycotoxin Exposure, Gut Health, and Impaired Growth: A Conceptual Framework. Adv Nutr. 2012; 3(4):526–531. DOI: https://doi.org/10.3945/an.112.002188
Hossain M, Nahar B, Haque MA, Mondal D, Mahfuz M, Naila NN, Gazi M, Hasan M, Haque N, Haque R, Arndt M, Walson J, Ahmed T. Serum Adipokines, Growth Factors, and Cytokines Are Independently Associated with Stunting in Bangladeshi Children. Nutrients. 2019; 11(8):1753. DOI: https://doi.org/10.3390/nu11081827
Xia X, Hao H, Zhang X, Wong IN, Chung SK, Chen Z, Xu B, Huang R. Immunomodulatory Sulfated Polysaccharides from Caulerpa racemosa var. peltata Induces Metabolic Shifts in NF-κB Signaling Pathway in RAW 264.7 Macrophages. Int J Biol Macromol. 2021; 182:321–332. DOI: https://doi.org/10.1016/j.ijbiomac.2021.04.025
Lucena AMM, Souza CRM, Jales JT, Guedes PMM, De Miranda GEC, de Moura AMA, Araujo-Junior J, Nascimento G, Scortecci K, Santos B, Souto J. The Bisindole Alkaloid Caulerpin, From Seaweeds of the Genus Caulerpa, Attenuated Colon Damage in Murine Colitis Model. Mar Drugs. 2018; 16(9):319. DOI: https://doi.org/10.3390/md16090318
Nagappan T and Vairappan CS. Nutritional and Bioactive Properties of Three Edible Species of Green Algae, Genus Caulerpa (Caulerpaceae). J Appl Phycol. 2014; 26(2):1019–1027. DOI: https://doi.org/10.1007/s10811-013-0147-8
Uebelhoer LS, Gwela A, Thiel B, Nalukwago S, Mukisa J, Lwanga C, Getonto J, Nyatichi E, Dena G, Makazi A, Mwaringa S, Mupere E, Berkley J, Lancioni C. Toll-Like Receptor-Induced Immune Responses During Early Childhood and Their Associations with Clinical Outcomes Following Acute Illness Among Infants in Sub-Saharan Africa. Front Immunol. 2022; 12:805216. DOI: https://doi.org/10.3389/fimmu.2021.748996
Sturgeon JP, Njunge JM, Bourke CD, Gonzales GB, Robertson RC, Bwakura-Dangarembizi M, Berkley J, Kelly P, Prendergast A. Inflammation: The Driver of Poor Outcomes Among Children with Severe Acute Malnutrition? Nutr Rev. 2023; 81(12):1636–1652. DOI: https://doi.org/10.1093/nutrit/nuad030
Dallakyan S and Olson AJ. Small-Molecule Library Screening by Docking with PyRx. In: Hempel JE, Williams CH, Hong CC, editors. Chemical Biology: Methods and Protocols. New York, NY: Springer New York; 2015:243–250. DOI: https://doi.org/10.1007/978-1-4939-2269-7_19
Zheng J, Xiong H, Li Q, He L, Weng H, Ling W, Wang D. Protocatechuic Acid from Chicory Is Bioavailable and Undergoes Partial Glucuronidation and Sulfation in Healthy Humans. Food Sci Nutr. 2019; 7(9):3071–3080. DOI: https://doi.org/10.1002/fsn3.1168
Zoete V, Daina A, Bovigny C, Michielin O. SwissSimilarity: A Web Tool for Low to Ultra High Throughput Ligand-Based Virtual Screening. J Chem Inf Model. 2016; 56(8):1399–1404. DOI: https://doi.org/10.1021/acs.jcim.6b00174
Yang M, Larson PG, Brown L, Schultz JR, Kucaba TA, Griffith TS, Ferguson D. Toll-Like Receptor 7 and 8 Imidazoquinoline-Based Agonist/Antagonist Pairs. Bioorg Med Chem Lett. 2022; 59:128548. DOI: https://doi.org/10.1016/j.bmcl.2022.128548
Keppler M, Straß S, Geiger S, Fischer T, Späth N, Weinstein T, Schwamborn A, Guezguez J, Guse J, Laufer S, Burnet M. Imidazoquinolines With Improved Pharmacokinetic Properties Induce a High IFNα to TNFα Ratio In Vitro and In Vivo. Front Immunol. 2023; 14:1143896. DOI: https://doi.org/10.3389/fimmu.2023.1168252
Rudik A, Bezhentsev V, Dmitriev A, Lagunin A, Filimonov D, Poroikov V. Metatox - Web Application for Generation of Metabolic Pathways and Toxicity Estimation. J Bioinform Comput Biol. 2019; 17(1):1940003. DOI: https://doi.org/10.1142/S0219720019400018
Guan L, Yang H, Cai Y, Sun L, Di P, Li W, Liu G, Tang Y. ADMET-Score - A Comprehensive Scoring Function for Evaluation of Chemical Drug-Likeness. Medchemcomm. 2019 Jan; 10(1):148–157. DOI: https://doi.org/10.1039/C8MD00472B
Discovery Studio 3.5. San Diego: Accelrys; 2017.
Lagunin A, Stepanchikova A, Filimonov D, Poroikov V. PASS: Prediction of Activity Spectra for Biologically Active Substances. Bioinformatics. 2000; 16(8):747–748. DOI: https://doi.org/10.1093/bioinformatics/16.8.747
Brown GJ, Cañete PF, Wang H, Medhavy A, Bones J, Roco JA, He Y, Qin Y, Cappelo J, Ellyard J, Bassett K, Shen Q, Burgio G, Zhang Y, Turnbull C, Meng X, Wu P, Cho E, Miosge L, Andrews T, Field M, Tvorogov D, Lopez A, Babon J, Lopez C, Gonzalez-Murillo A, Garulo D, Pascual V, Levy T, Mallack E, Calame D, Lotze T, Lupski J, Ding H, Ullah T, Walters G, Koina K, Cook M, Shen N, de Lucas Collantes C, Corry B, Gantier M, Athanasopoulos V, Vinuesa C. TLR7 Gain-of-Function Genetic Variation Causes Human Lupus. Nature. 2022; 605(7909):349–356. DOI: https://doi.org/10.1038/s41586-022-04642-z
Zheng H, Wu P, Bonnet PA. Recent Advances on Small-Molecule Antagonists Targeting TLR7. Molecules. 2023; 28(2):494. DOI: https://doi.org/10.3390/molecules28020634
Patinote C, Karroum NB, Moarbess G, Cirnat N, Kassab I, Bonnet PA, Deleuze-Masquefa C. Agonist and Antagonist Ligands of Toll-Like Receptors 7 and 8: Ingenious Tools for Therapeutic Purposes. Eur J Med Chem. 2020; 193:112238. DOI: https://doi.org/10.1016/j.ejmech.2020.112238
Zhang Z, Ohto U, Shibata T, Taoka M, Yamauchi Y, Sato R, Shukla N, David S, Isobe T, Miyake K, Shimizu T. Structural Analyses of Toll-Like Receptor 7 Reveal Detailed RNA Sequence Specificity and Recognition Mechanism of Agonistic Ligands. Cell Rep. 2018; 25(12):3371–3381.e5. DOI: https://doi.org/10.1016/j.celrep.2018.11.081
National Center for Biotechnology Information. PubChem Compound Summary for CID 10309114, Cpg-52852. National Center for Biotechnology Information. 2025. Available from: https://pubchem.ncbi.nlm.nih.gov/compound/Cpg-52852
Engel AL, Holt GE, Lu H. The Pharmacokinetics of Toll-Like Receptor Agonists and the Impact on the Immune System. Expert Rev Clin Pharmacol. 2011; 4(2):275–289. DOI: https://doi.org/10.1586/ecp.11.5
Järvinen E, Deng F, Kiander W, Sinokki A, Kidron H, Sjöstedt N. The Role of Uptake and Efflux Transporters in the Disposition of Glucuronide and Sulfate Conjugates. Front Pharmacol. 2022; 12:822452. DOI: https://doi.org/10.3389/fphar.2021.802539
Docampo-Palacios ML, Alvarez-Hernández A, Adiji O, Gamiotea-Turro D, Valerino-Diaz AB, Viegas LP, Ndukwe I, De Fatima A, Heiss C, Azadi P, Pasinetti G, Dixon R. Glucuronidation of Methylated Quercetin Derivatives: Chemical and Biochemical Approaches. J Agric Food Chem. 2020; 68(50):14790–14807. DOI: https://doi.org/10.1021/acs.jafc.0c04500
Vitku J, Hill M, Kolatorova L, Kubala Havrdova E, Kancheva R. Steroid Sulfation in Neurodegenerative Diseases. Front Mol Biosci. 2022; 9:827018. DOI: https://doi.org/10.3389/fmolb.2022.839887
Liang SC, Xia YL, Hou J, Ge GB, Zhang JW, He YQ, Wang J, Qi X, Yang L. Methylation, Glucuronidation, and Sulfonation of Daphnetin in Human Hepatic Preparations In Vitro: Metabolic Profiling, Pathway Comparison, and Bioactivity Analysis. J Pharm Sci. 2016; 105(2):808–816. DOI: https://doi.org/10.1016/j.xphs.2015.10.010
Teles YCF and De Souza MSFV. Sulphated Flavonoids: Biosynthesis, Structures, and Biological Activities. Molecules. 2018; 23(2):475. DOI: https://doi.org/10.3390/molecules23020480
Williamson G, Kay CD, Crozier A. The Bioavailability, Transport, and Bioactivity of Dietary Flavonoids: A Review from a Historical Perspective. Compr Rev Food Sci Food Saf. 2018; 17(15):1054–1112. DOI: https://doi.org/10.1111/1541-4337.12351
Balansa W, Riyanti, Balansa KH, Hanif N. Harnessing the Ecofriendly Antifouling Potential of Agelasine Alkaloids Through MetaTox Analysis and Computational Studies. Trop J Nat Prod Res. 2025; 9(1):329–340. DOI: https://doi.org/10.26538/tjnpr/v9i1.42
Balansa W, Rieuwpassa FJ, Hanif N. Harnessing Ecofriendly Antifouling of Agelasine Alkaloids. Kamiya Jaya Aquatic; 2025.
Wang KP, Neumann C, Epp A, Zeng W, Griffith T, Ferguson D, Gardai S, Smith A. Generation of an Antibody-Drug Conjugate-Optimized TLR 7/8 Agonist Payload. Cancer Res. 2023; 83(7 Suppl):1542–1542. DOI: https://doi.org/10.1158/1538-7445.AM2023-1542
Tojo S, Zhang Z, Matsui H, Tahara M, Ikeguchi M, Kochi M, Kamada M, Shigematsu H, Tsutsumi A, Adachi N, Shibata T, Yamamoto M, Kikkawa M, Senda T, Isobe Y, Ohto U, Shimizu T. Structural Analysis Reveals TLR7 Dynamics Underlying Antagonism. Nat Commun. 2020; 11(1):5015. DOI: https://doi.org/10.1038/s41467-020-19025-z
Ohto U, Tanji H, Shimizu T. Structure and Function of Toll-Like Receptor 8. Microbes Infect. 2014; 16(4):273–282. DOI: https://doi.org/10.1016/j.micinf.2014.01.007
Gies JP and Landry Y. 4 - Drug Targets: Molecular Mechanisms of Drug Action. In: Wermuth CG, editor. The Practice of Medicinal Chemistry (Second Edition). London: Academic Press; 2003:51–65. DOI: https://doi.org/10.1016/B978-012744481-9/50008-8
Ishizaka ST, Hawkins L, Chen Q, Tago F, Yagi T, Sakaniwa K, Zhang Z, Shimizu T, Shirato M. A Novel Toll-Like Receptor 7/8–Specific Antagonist E6742 Ameliorates Clinically Relevant Disease Parameters in Murine Models of Lupus. Eur J Pharmacol. 2023; 957:175962. DOI: https://doi.org/10.1016/j.ejphar.2023.175962
Chiney M, Girgis I, Harrison M, Zhang X, Shen Y, Dawes M, Dong L, Shevell D, Aras U, Murthy B. BMS-986256, an Oral Novel Toll-Like Receptor 7 and 8 (TLR7/8) Inhibitor, Does Not Affect the Pharmacokinetics of Mycophenolate Mofetil in Healthy Subjects. Arthritis Rheumatol. 2021; 73(9):3686–3688.
Weeratna RD, Makinen SR, McCluskie MJ, Davis HL. TLR Agonists as Vaccine Adjuvants: Comparison of CpG ODN and Resiquimod (R-848). Vaccine. 2005; 23(45):5263–5270. DOI: https://doi.org/10.1016/j.vaccine.2005.06.024
Hu A, Sun L, Lin H, Liao Y, Yang H, Mao Y. Harnessing Innate Immune Pathways for Therapeutic Advancement in Cancer. Signal Transduct Target Ther. 2024; 9(1):68. DOI: https://doi.org/10.1038/s41392-024-01765-9
Chen CJ, Jiang C, Yuan J, Chen M, Cuyler J, Xie XQ, Feng Z. How Do Modulators Affect the Orthosteric and Allosteric Binding Pockets? ACS Chem Neurosci. 2022; 13(7):959–977. DOI: https://doi.org/10.1021/acschemneuro.1c00749
Tanji H, Ohto U, Shibata T, Miyake K, Shimizu T. Structural Reorganization of the Toll-Like Receptor 8 Dimer Induced by Agonistic Ligands. Science (1979). 2013; 339(6126):1426–1429. DOI: https://doi.org/10.1126/science.1229159
Patra MC, Achek A, Kim GY, Panneerselvam S, Shin HJ, Baek WY, Lee W, Sung J, Jeong U, Cho E, Kim W, Kim E, Suh C, Choi S. A Novel Small-Molecule Inhibitor of Endosomal TLRs Reduces Inflammation and Alleviates Autoimmune Disease Symptoms in Murine Models. Cells. 2020; 9(7):1676. DOI: https://doi.org/10.3390/cells9071648