Chitosan Nanoparticles as a Therapeutic Agent for Mitigating Paracetamol-Induced Liver Damage in White Male Albino Rats
Main Article Content
Abstract
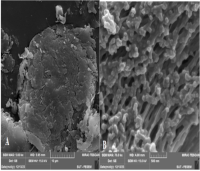
High paracetamol doses can cause liver damage, but chitosan nanoparticles (ChNPs), known for their biocompatibility, biodegradability, anti-inflammatory, and antioxidant properties, may offer potential therapeutic benefits. This study investigated the protective effects of ChNPs in mitigating paracetamol-induced liver damage in white male albino rats. Chitosan nanoparticles were synthesized and characterized using scanning electron microscopy, atomic force microscopy, and UV-Vis spectroscopy. Sixty adult male white albino rats (200–250 g) were randomly assigned to six groups and treated orally for three months. Groups received distilled water (Group I), 15 mg/kg ChNPs (Group II), 500 mg/kg (Group III), or 1000 mg/kg (Group IV) paracetamol or combinations of 500 mg/kg (Group V) or 500 mg/kg (Group VI) paracetamol with 15 mg/kg ChNPs. Liver tissues were histologically examined, and DNA damage was assessed. The results showed that ChNPs (43–80 nm) exhibited smooth, spherical morphology with improved dispersion. Prolonged oral administration of paracetamol at both doses induced significant histopathological changes, including fibrosis, congestion, and inflammatory infiltration in liver tissues. Co-administration with ChNPs preserved liver architecture, reducing morphological abnormalities. The comet assay showed significant DNA strand breaks in paracetamol-treated rats, indicated by increased tail DNA% and tail length. Chitosan nanoparticles mitigated DNA damage, likely due to their antioxidant and anti-inflammatory properties. The study’s findings revealed that ChNPs exhibited a protective effect against paracetamol-induced hepatotoxicity, mitigating both histopathological and genetic alterations. These findings underscore the potential therapeutic application of ChNPs in preventing drug-induced liver damage and support their broader use in nanomedicine.
Downloads
Article Details
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
How to Cite
References
1.Sharma CV, Mehta V. Paracetamol: mechanisms and updates. Contin Educ Anaesth Crit Care Pain. 2014;14(4):153–158.
2.Majeed S, Ramadhan M, Monther W. Long-term toxicological effects of paracetamol in rats. Iraqi J Vet Sci. 2013;27(1):65–70.
3.Kumar AS, Ramadas A, Selvam SP, Selvaraj S. A review of recent advancements in nanotechnology for medical drugs delivery. Res J Pharm Technol. 2024;17(4):1891–4.
4.Javed B, Ikram M, Farooq F, Sultana T, Mashwani ZU, Raja NI. Biogenesis of silver nanoparticles to treat cancer, diabetes, and microbial infections: a mechanistic overview. Appl Microbiol Biotechnol. 2021;105(6):2261-2275.
5.Sumaila A, Idris SO, Musa A, Ajibola VO. Extraction and characterization of chitosan from crab shells: kinetic and thermodynamic studies of arsenic and copper adsorption from electroplating wastewater. Iraqi J Sci. 2020;2156–2171.
6.Aranaz I, Alcántara AR, Civera MC, Arias C, Elorza B, Heras Caballero A, Acosta N. Chitosan: An overview of its properties and applications. Polymers (Basel). 2021;13(19):3256.
7.Matty FS, MohiALDeen ZM. Swelling behavior and drug release of interpenetrating network composed of PVA and chitosan. Ibn AL-Haitham J Pure Appl Sci. 2018;31(1):145–156.
8.Jha R, Mayanovic RA. A review of the preparation, characterization, and applications of chitosan nanoparticles in nanomedicine. Nanomat (Basel). 2023;13(8):1302.
9.Younus MA, Abdallaha BF. Synthesis, characterization and anticancer activity of chitosan Schiff base/PVP gold nanocomposite in treating esophageal cancer cell line. Baghdad Sci J. 2024;21(1):0095.
10.Mohsen AH, Ali NA. Improve wettability of polycaprolactone (PCL)/chitosan of wound dressings by plasma jet. Iraqi J Sci. 2022;4761–4770.
11.Kadhum WN, Al-Ogaidi IAZ. Evaluation of chitosan-alginate nanoparticle as a stable antibacterial formula in biological fluids. Iraqi J Sci. 2022;2398–2418.
12.Mian P, Allegaert K, Spriet I, Tibboel D, Petrovic M. Paracetamol in older people: towards evidence-based dosing? Drugs Aging. 2018;35(7):603-624.
13.Al-Doaiss AA. Hepatotoxicity-induced by the therapeutic dose of acetaminophen and the ameliorative effect of oral co-administration of selenium/Tribulus terrestris extract in rats. Int J Morphol. 2020;38(5):1444–1454.
14.Jackson P, Pedersen LM, Kyjovska ZO, Jacobsen NR, Saber AT, Hougaard KS, Vogel U, Wallin H. Validation of freezing tissues and cells for analysis of DNA strand break levels by comet assay. Mutagenesis. 2013;28(6):699-707.
15.Araujo JM, Fortes-Silva R, Pola CC, Yamamoto FY, Gatlin DM 3rd, Gomes CL. Delivery of selenium using chitosan nanoparticles: Synthesis, characterization, and antioxidant and growth effects in Nile tilapia (Orechromis niloticus). PLoS One. 2021;16(5):e0251786.
16.Salman Z, Alwash BM, Kadhim E. Isolation and identification of flavonoid compounds from Euphorbia milii plant cultivated in Iraq and evaluation of its genetic effects on two types of cancer cell line. Baghdad Sci J. 2024; 21(9):2805-2819.
17.Kain D, Kumar S. Synthesis and characterization of chitosan nanoparticles of Achillea millefolium L. and their activities. F1000Research. 2020;9:1297.
18.Mnati IM, Mutlak BH. Histopathological changes in liver induced by piroxicam administration in adult male albino mice Mus musculus. Indian J Forensic Med Toxicol. 2020;14(3): 1535-1541.
19.Kim SH, Choi HJ, Seo H, Kwon D, Yun J, Jung YS. Downregulation of glutathione-mediated detoxification capacity by binge drinking aggravates acetaminophen-induced liver injury through IRE1α ER stress signaling. Antioxidants (Basel). 2021;10(12):1949.
20.Diab KA, Fahmy MA, Hassan EM, Hassan ZM, Omara EA, Abdel-Samie NS. Inhibitory activity of black mulberry (Morus nigra) extract against testicular, liver and kidney toxicity induced by paracetamol in mice. Mol Biol Rep. 2020;47(3):1733-1749.
21.Ramachandran A, Jaeschke H. Oxidant stress and acetaminophen hepatotoxicity: mechanism-based drug development. Antioxid Redox Signal. 2021;35(9):718-733.
22.Rotundo L, Pyrsopoulos N. Liver injury induced by paracetamol and challenges associated with intentional and unintentional use. World J Hepatol. 2020;12(4):125-136.
23.de Sousa Victor R, Marcelo da Cunha Santos A, Viana de Sousa B, de Araújo Neves G, Navarro de Lima Santana L, Rodrigues Menezes R. A Review on chitosan's uses as biomaterial: tissue engineering, drug delivery systems and cancer treatment. Materials (Basel). 2020;13(21):4995.
24.Wijesekara T, Xu B. New Insights into Sources, Bioavailability, Health-Promoting Effects, and Applications of Chitin and Chitosan. J Agric Food Chem. 2024;72(31):17138-17152.
25.Herdiana Y, Wathoni N, Shamsuddin S, Muchtaridi M. Drug release study of the chitosan-based nanoparticles. Heliyon. 2021;8(1):e08674.
26.Aibani N, Rai R, Patel P, Cuddihy G, Wasan EK. Chitosan nanoparticles at the biological interface: implications for drug delivery. Pharmaceutics. 2021;13(10):1686.
27.McGill MR, Williams CD, Xie Y, Ramachandran A, Jaeschke H. Acetaminophen-induced liver injury in rats and mice: comparison of protein adducts, mitochondrial dysfunction, and oxidative stress in the mechanism of toxicity. Toxicol Appl Pharmacol. 2012;264(3):387-94.
28.Karayianni M, Sentoukas T, Skandalis A, Pippa N, Pispas S. Chitosan-based nanoparticles for nucleic acid delivery: technological aspects, applications, and future perspectives. Pharmaceutics. 2023 ;15(7):1849.
29.Dawoud SF, Al-Akra TM, Zedan AM. Hepatoprotective effects of chitosan and chitosan nanoparticles against biochemical, genetic, and histological disorders induced by the toxicity of emamectin benzoate. Rep Biochem Mol Biol. 2021;10(3):506-514.