Biopolymer Nanoencapsulation of Andrographis paniculata (Burm. f.) Nees and Carboxymethyl Chitosan for Dengue Therapy
Main Article Content
Abstract
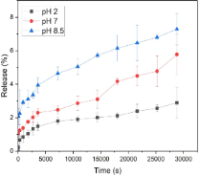
Dengue fever is a global health problem, with millions of cases reported each year. The lack of available therapeutic agents has stimulated the search for new treatments. This study aimed to synthesize, and characterize biopolymer-based nanoencapsules using Andrographis paniculata and carboxymethyl chitosan (CMC), and evaluate their activity against dengue virus. A. paniculata nanocapsules (AP-NPs) were formulated by ultrasonication of A. paniculata extract with carboxymethyl chitosan. AP-NPs were characterized by particle size analysis, Fourier Transform Infrared (FTIR) analysis, and stability under various conditions of pH, temperature, and electrolyte (NaCl). The antiviral activity against dengue virus (DENV-2), and cytotoxic activity against Vero cell line were evaluated according to standard procedures. AP-NPs was successfully synthesized with particle size of 305.5 ± 30.12 nm, and a polydispersity index (PDI) of 0.3319 ± 0.01. AP-NPs had improved stability and better controlled release of bioactive components than A. paniculata extract. AP-NPs had a loading amount of 27.18 ± 2.51%, and a loading efficiency of 54.36 ± 5.02%. AP-NPs exhibited enhanced antiviral activity and bioavailability compared to the pure A. paniculata extract, although with increased cytotoxicity. The CC₅₀ of AP-NPs was 734.56 μg/mL, which was significantly lower than that of the extract (1522.95 μg/mL), while the EC₅₀ for AP-NPs was 68.12 μg/mL, compared to 9.87 μg/mL for the extract. Despite the higher toxicity, AP-NPs offer promising potential as a therapeutic candidate for dengue fever, particularly due to their ability to improve bioavailability and provide sustained antiviral effects.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
How to Cite
References
1. European Centre for Disease Prevention and Control. Dengue Worldwide Overview. [Internet]. Available from: https://ecdc.europa.eu/en/dengue-monthly [Accessed Dec 12, 2024].
2. Zerfu B, Kassa T, Legesse M. Epidemiology, biology, pathogenesis, clinical manifestations, and diagnosis of dengue virus infection, and its trend in Ethiopia: A comprehensive literature review. Trop Med Health. 2023; 51(1):11. https://doi.org/10.1186/s41182-023-00504-0.
3. Amorim MT, Hernández LH, Naveca FG, Essashika Prazeres IT, Wanzeller ALM, Silva EVPD, Casseb LMN, Silva FSD, da Silva SP, Nunes BTD, Cruz ACR. Emergence of a new strain of DENV-2 in South America: Introduction of the cosmopolitan genotype through the Brazilian-Peruvian border. Trop Med Infect Dis. 2023;8(6):325. https://doi.org/10.3390/tropicalmed8060325.
4. Kok BH, Lim HT, Lim CP, Lai NS, Leow CY, Leow CH. Dengue virus infection—a review of pathogenesis, vaccines, diagnosis, and therapy. Virus Res. 2023; 324:199018. https://doi.org/10.1016/j.virusres.2022.199018.
5. Pajor MJ, Long B, Liang SY. Dengue: A focused review for the emergency clinician. Am J Emerg Med. 2024; 82:82–87. https://doi.org/10.1016/j.ajem.2024.05.022.
6. Wardana AP, Aminah NS, Kristanti AN, Fahmi MZ, Abdjan MI, Teguh H. Species used as herbal medicine in Indonesia. Trop J Nat Prod Res. 2024; 8(9):8393–8399. https://doi.org/10.26538/tjnpr/v8i9.22.
7. Rafi M, Karomah AH, Heryanto R, Septaningsih DA, Kusuma WA, Amran MB, Rohman A, Prajogo B. Metabolite profiling of Andrographis paniculata leaves and stem extract using UHPLC-Orbitrap-MS/MS. Nat Prod Res. 2022; 36(2):625–629. https://doi.org/10.1080/14786419.2020.1789637.
8.Irawan C, Enriyani R, Ismail, Sukiman M, Putri ID, Utami A, Rahmatia L, Lisandi A. Effects of solvent variation on the antioxidant, anti-inflammatory, and alpha-glucosidase inhibitory activity of Andrographis paniculata leaves extract. Trop J Nat Prod Res. 2024; 8(1):5968–5972. https://doi.org/10.26538/tjnpr/v8i1.36.
9. Ramalingam S, Karupannan S, Padmanaban P, Vijayan S, Sheriff K, Palani G, Krishnasamy KK. Anti-dengue activity of Andrographis paniculata extracts and quantification of dengue viral inhibition by SYBR Green reverse transcription polymerase chain reaction. Ayu. 2018; 39(2):87–91. https://doi.org/10.4103/ayu.AYU_144_17.
10. Nguyen HT, Do VM, Phan TT, Nguyen Huynh DT. The potential of ameliorating COVID-19 and sequelae from Andrographis paniculata via bioinformatics. Bioinform Biol Insights. 2023;17: 11779322221149622. https://doi.org/10.1177/11779322221149622.
11. Intharuksa A, Arunotayanun W, Yooin W, Sirisa-ard P. A comprehensive review of Andrographis paniculata and its constituents as potential lead compounds for COVID-19 drug discovery. Molecules. 2022; 27(14): 4479. https://doi.org/10.3390/molecules27144479.
12. Dewi BE, Desti H, Ratningpoeti E, Sudiro M, Fithriyah, Angelina M. Effectivity of quercetin as antiviral to dengue virus-2 strain New Guinea C in Huh 7-It 1 cell line. IOP Conf Ser Earth Environ Sci. 2020; 462(1):012033. https://doi.org/10.1088/1755-1315/462/1/012033.
13. Sun D, Gao W, Hu H, Zhou S. Why 90% of clinical drug development fails and how to improve it? Acta Pharm Sin B. 2022; 12(7):3049–3062. https://doi.org/10.1016/j.apsb.2022.02.002.
14. Hua S. Advances in oral drug delivery for regional targeting in the gastrointestinal tract—influence of physiological, pathophysiological, and pharmaceutical factors. Front Pharmacol. 2020; 11:1–22. https://doi.org/10.3389/fphar.2020.00524.
15. Delshadi R, Bahrami A, McClements DJ, Moore MD, Williams L. Development of nanoparticle-delivery systems for antiviral agents: A review. J Control Release. 2021; 331:30–44. https://doi.org/10.1016/j.jconrel.2021.01.017.
16. Cahyaningrum SE, Amaria, Muhaimin FI. The kinetic release and in-vivo study of alginate-chitosan encapsulated metformin against type II diabetes mellitus. Rasayan J Chem. 2022;15(2):1040–1044. https://doi.org/10.31788/RJC.2022.1526763.
17. Ravi H, Kurrey N, Manabe Y, Sugawara T, Baskaran V. Polymeric chitosan-glycolipid nanocarriers for an effective delivery of marine carotenoid fucoxanthin for induction of apoptosis in human colon cancer cells (Caco-2 cells). Mater Sci Eng C Mater Biol Appl. 2018; 91:785–797. https://doi.org/10.1016/j.msec.2018.06.018.
18. Costa JR, Xavier M, Amado IR, Gonçalves C, Castro PM, Tonon RV, Cabral LMC, Pastrana L, Pintado ME. Polymeric nanoparticles as oral delivery systems for a grape pomace extract towards the improvement of biological activities. Mater Sci Eng C. 2021; 119:111551. https://doi.org/10.1016/j.msec.2020.111551.
19. Jafernik K, Ładniak A, Blicharska E, Czarnek K, Ekiert H, Wiącek AE, Szopa A. Chitosan-based nanoparticles as effective drug delivery systems—a review. Molecules. 2023; 28(4):1963. https://doi.org/10.3390/molecules28041963.
20. Suryani S, Chaerunisaa AY, Joni IM, Ruslin R, Aspadiah V, Anton A, Sartinah A, Ramadhan OAN. The chemical modification to improve solubility of chitosan and its derivatives: application, preparation method, toxicity as a nanoparticle. Nanotechnol Sci Appl. 2024;17:41–57. https://doi.org/10.2147/NSA.S450026.
21. Azman M, Sabri AH, Anjani QK, Mustaffa MF, Hamid KA. Intestinal absorption study: challenges and absorption enhancement strategies in improving oral drug delivery. Pharmaceuticals. 2022;15(8):975. https://doi.org/10.3390/ph15080975.
22. Tobias A and Sadiq NM. Physiology, gastrointestinal nervous control; In StatPearls [Internet]. StatPearls Publishing: Treasure Island (FL); 2024. PMID: 31424852..
23. Liu Y, Sun M, Wang T, Chen X, Wang H. Chitosan-based self-assembled nanomaterials: their application in drug delivery. View. 2021; 2(1):1-13. https://doi.org/10.1002/VIW.20200069.
24. Noore S, Rastogi NK, O’Donnell C, Tiwari B. Novel bioactive extraction and nano-encapsulation. Encyclopedia. 2021; 1(3):632–664. https://doi.org/10.3390/encyclopedia1030052
25. Wardana AP, Aminah NS, Novi A, Kristanti A, Manuhara YSW, Fahmi MZ, Sucipto TH, Abdjan MI, Indriani. Gynura procumbens nanoencapsulation: A novel promising approach to combat dengue infection. Rasayan J Chem. 2023;16(2):0976–0983. https://doi.org/10.31788/rjc.2023.1628298.
26. Kalliola S, Repo E, Srivastava V, Zhao F, Heiskanen JP, Sirviö JA, Liimatainen H, Sillanpää M. Carboxymethyl chitosan and its hydrophobically modified derivative as pH-switchable emulsifiers. Langmuir. 2018;34(8):2800–2806. https://doi.org/10.1021/acs.langmuir.7b03959.
27. Sucipto TH, Setyawati H, Churrotin S, Amarullah IH, Sumarsih S, Wardhani P, Aryati A, Soegijanto S. Anti-dengue type 2 virus activities of zinc (II) complex compounds with 2-(2,4-dihydroxyphenyl)-3,5,7-trihydroxycromen-4-one ligands in Vero cells. Indones J Trop Infect Dis. 2019;7(5):105. https://doi.org/10.20473/ijtid.v7i5.10851.
28. Khan I, Saeed K, Khan I. Nanoparticles: properties, applications, and toxicities. Arab J Chem. 2019; 12(7):908–931. https://doi.org/10.1016/j.arabjc.2017.05.011.
29. Danaei M, Dehghankhold M, Ataei S, Hasanzadeh Davarani F, Javanmard R, Dokhani A, Khorasani S, Mozafari MR. Impact of particle size and polydispersity index on the clinical applications of lipidic nanocarrier systems. Pharmaceutics. 2018; 10(2):87. https://doi.org/10.3390/pharmaceutics10020057.
30. Koshani R and Jafari SM. Ultrasound-assisted preparation of different nanocarriers loaded with food bioactive ingredients. Adv Colloid Interface Sci. 2019; 270:123–146. https://doi.org/10.1016/j.cis.2019.06.005.
31. Pateiro M, Gómez B, Munekata PES, Barba FJ, Putnik P, Kovačević DB, Lorenzo JM. Nanoencapsulation of promising bioactive compounds to improve their absorption, stability, functionality, and the appearance of the final food products. Molecules. 2021; 26(6):1547. https://doi.org/10.3390/molecules26061547.
32. Ambati R, Kho LK, Prentice D, Thompson A. Osmotic demyelination syndrome: novel risk factors and proposed pathophysiology. Intern Med J. 2023; 53(7):1154–1162. https://doi.org/10.1111/imj.15855.
33. Buffington MA and Abreo K. Hyponatremia: a review. J Intensive Care Med. 2016; 31(4):223–236. https://doi.org/10.1177/0885066614566794.
34. Nishida K, Morita H, Katayama Y, Inoue R, Kanaya T, Sadakane K, Seto H. Salting-out and salting-in effects of amphiphilic salt on cloud point of aqueous methylcellulose. Process Biochem. 2017; 59:52–57. https://doi.org/10.1016/j.procbio.2016.12.009.
35. Nugraheni PS, Soeriyadi AH, Sediawan WB, Ustadi, Budhijanto W. Influence of salt addition and freezing-thawing on particle size and zeta potential of nano-chitosan. IOP Conf Ser Earth Environ Sci. 2019; 278(1):012052. https://doi.org/10.1088/1755-1315/278/1/012052.