Effect of Vitamin D3 on Hormonal and Histological Changes in Thyroid Gland Caused by Hyperprolactinemia of Male laboratory Rats (Rattus norvegicus) http://www.doi.org/10.26538/tjnpr/v7i8.9
Main Article Content
Abstract
Hyperprolactinemia is commonly known as abnormal levels of prolactin hormone in the blood due to endocrine disorder. The study aimed to eliminate hyperprolactinemia affecting the thyroid gland by treating it with vitamin D supplements. Eighteen male rats Rattus norvegicus were divided into three groups of six rats each : The first group received normal saline for 42 days . The second group, rats were given 5 mg/kg metoclopramide by intraperitoneal injection for hyperprolactinemia induction for 14 days. The third group, hyperprolactinemic rats received 2.5 mg/kg vitamin D3 by intraperitoneal injection for 28 days. After the end of experimental )42 days(,
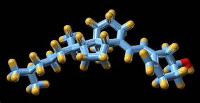
hormonal parameters (prolactin hormone, Triiodothyronine hormone )T3(, and Thyroxine hormone) T4) , Thyroid stimulating hormone )TSH( were measure, and the thyroid gland was removed, processed and examine for histomorphological changes. The result of the study revealed a significant decrease (P≤0.01) in prolactin and TSH levels and a significant increase (P≤0.01) in T3 and T4 levels in Group 3 )Hyperprolactinemia group treated with vitamin D ( compared with Group 2 ) Hyperprolactinemia group(. Histological examination of sections of the thyroid gland of the group treated with vitamin D3 showed significant restoration compared to the hyperprolactinemia rats, throughout. Thyroid follicles became larger, containing dense colloidal material, in the group given Vitaim D 3 and structures of thyroid follicles. The study concluded that vitamin D3 had a protective effect on thyroid gland by stabilizing T3, T4, and TSH hormones
levels and restoration of histological architectures and thyroid follicles became larger, containing dense colloidal material, with presence normal thyrocytes remarkably.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
Halperin RI, Cámara GR, García MM, Ollero GD. Clinical guidelines for diagnosis and treatment of prolactinoma and hyperprolactinemia. Endocrinologíay Nutrición (English Edition). 2013; 60(6): 308–319.
Hoskova K, Bryant N K, Chen ME, Nachtigall L B, Lippincott M F, Balasubramanian R, Seminara SB. Kisspeptin Overcomes GnRH Neuronal Suppression Secondary to Hyperprolactinemia in Humans. Journal of Clinical Endocrinology and Metabolism. 2022; 107(8) : 3515–3525.
Zeng Y, Huang Q, Zou Y, Tan J, Zhou W, Li M. The efficacy and safety of quinagolide in hyperprolactinemia treatment: A systematic review and meta-analysis. Frontiers in Endocrinology. 2023; 1- 14
Tomova N, & Pharmacist C. Guidance on the Treatment of Antipsychotic Induced Hyperprolactinaemia in Adults Version 1. NHS Foundation Trust, 2016; 623349:2–9.
Vilar L, Vilar CF, Lyra R, Da Conceição Freitas M. Pitfalls in the Diagnostic Evaluation of Hyperprolactinemia. Neuroendocrinology. 2019; 109(1):7–19.
McCallum R W, Sowers J R, Hershman J M, Sturdevant R A L. Metoclopramide stimulates prolactin secretion in man. Journal of Clinical Endocrinology and Metabolism. 1976; 42(6), 1148–1152. https://doi.org/10.1210/jcem-42-6-1148
ABRAHEM N N, DREIJ S H, Al-Deresawi M S. Synergism of Hypothyroidism and Hyperprolactinemia to impact on efficiency of menstrual cycle and ovulatory status. Journal of Education College Wasit University, 2017; 1(28), 661–670.
Kim D. The role of vitamin D in thyroid diseases. Int. J of Mol Sci. 2017; 18(9): 1–19
Šošić-Jurjević B, Trifunović S, Živanović J, Ajdžanović V, Miler M, Ristić N, Filipović B. Vitamin D3 Treatment Alters Thyroid Functional Morphology in Orchidectomized Rat Model of Osteoporosis. International Journal of Molecular Sciences, (2022);23(1-16).
Sluczanowska-Glabowska S, Laszczynska M, Wylot M, Glabowski W, Piasecka M, Gacarzewicz D. Morphological and immunohistochemical compare of three rat prostate lobes (lateral, dorsal and ventral) in experimental hyperprolactinemia. Folia Histochemica et Cytobiologica,
(2010); 48(3),( 447-454).
Yin Y, Yu Z, Xia M, Luo X, Lu X, Ling W. Vitamin D attenuates high fat diet-induced hepatic steatosis in rats by modulating lipid metabolism. European Journal of Clinical Investigation. 2012; 42(11) : 1189–1196.
Bancroft, J, D. and Gamble, M. (2008). Theory and practices of histological technique. 2 and ed. Churchill Elseirier. London., Pp: 56.
Mahmoud, E. A., Al-Bakri, N. A., & Qasim, B. J. (2018). Histopathological changes of placenta in pregnant women complicated with pregestational diabetes. Journal of Pharmaceutical Sciences and Research, 10(11), 2952-2959.
Inche A G, Thangue N B. Keynote review: Chromatin control and cancer-drug discovery: realizing the promise. Drug discovery today. 2006; 11(3-4): 97-109.
Serri O, Chik C L, Ur E, Ezzat S. Diagnosis and management of hyperprolactinemia. Cma. 2003; 169(6) : 575-581.
Ahi S, Dehdar M R, Hatami N. Vitamin D deficiency in nonautoimmune hypothyroidism: A case-control study. BMC Endocrine Disorders. 2020; 20(1) : 4–9.
Appunni S, Rubens M, Ramamoorthy V, Saxena A, Tonse R, Veledar E, McGranaghan P. Association between vitamin D deficiency and hypothyroidism: results from the National Health and Nutrition Examination Survey (NHANES) 2007–2012. BMC Endocrine Disorders. 2021; 21(1) : 1–9.
Murdoch G H, Rosenfeld M G. Regulation of pituitary function and prolactin production in the GH4 cell line by vitamin D. J of Biol Chem. 1981; 256(8) : 4050–4055.
Miteva M Z, Nonchev BI, Orbetzova M M, Stoencheva SD. Vitamin D and Autoimmune Thyroid Diseases - a Review. Folia Medica. 2020; 62(2) : 223–229.
El-desouki N I, Salem M L, Mohamed IH, Nasef M, Abdallah FM. Hyperprolactinemia induced histological alterations in mice adrenal glands. 2018; 9(1-5)