Leucocyte Counts and Derivatives as Inflammatory Indicators in Active Tuberculosis http://www.doi.org/10.26538/tjnpr/v7i5.30
Main Article Content
Abstract
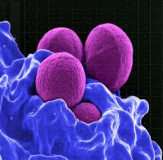
Tuberculosis (TB) is a disease of public health concern in Nigeria as the country is listed among the 30 high TB burden countries in the world. It is caused by Mycobacterium tuberculosis, an airborne pathogen. Tuberculosis disease is a manifestation of an active state of the infection when host immune response has been overwhelmed. Leucocytes participate in immune response, and traditionally, the total and differential counts have been useful in offering general outlook on inflammation as well as immunodeficiency. Lately, leucocyte derivatives such as neutrophil-tolymphocyte ratio (NLR) and lymphocyte-monocyte ratio (LMR) have been reported as better
markers of inflammation in some disease conditions. This study assessed total and differential leucocyte counts together with the derivatives in active tuberculosis infection among 80 tuberculosis patients and equal number of matched controls. Total and differential leucocyte counts were determined using standard haematology autoanalyzer, while the ratios were mathematically derived. Data were analyzed and hypotheses tested using student’s t-test on statistical package for social sciences (SPSS) version 21. A p-value of ≤0.05 was considered as statistically significant. Neutrophil-lymphocyte ratio was significantly higher in TB patients,
while lymphocyte-monocyte ratio was significantly lower in TB patients than the control. Furthermore, neutrophil-lymphocyte ratio was significantly higher, while the lymphocytemonocyte ratio was significantly lower in TB patients at diagnosis (n=26) in comparison with
those on treatment (n=54). There is derangement in leucocyte derivatives in association with tuberculosis. These derivatives improved significantly as anti-TB treatment progressed. Therefore, these variables could serve as useful indicators in the monitoring of treatment for TB patients.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
World Health Organization. Global TB Report 2020. Available from https://www.who.int › teams › tb-reports. Accessed 15th September, 2022.
World Health Organization. Global TB Report 2021. Available from https://www.who.int › teams › tb-reports. Accessed 8th November, 2022
Najecha TI, Rabia H, Rirdaus S, Ghaffer D. Association of plasma cytokines with radiological recover in pulmonary tuberculosis patients: Int J Mycobacteriol. 2016; 5 :111-119.
Levinson W, Chin-Hong P, Nussbaum J, Schwartz BS. Review of Medical Microbiology & immunology: a guide to clinical infectious diseases 16th ed. McGraw-Hill Education 2020.
Hoffbrand AV, Steensma DP. Hoffbrand’s Essential Haematology 8th ed. Willey-Blackwell 2019; pp 423.
Ermert D, Niemiec MJ, Röhm M, Glenthoj A, Borregard N, Urban CF. Candida albicans escapes mouse neutrophils. J. Leukoc. Biol. 2013; 94(2):223-236.
Barer MR. The natural history of infection. Medical Microbiology. Elsevier, Netherlands 2012.
Yoo SK, Starnes TW, Deng Q, Huttenlocher A. Lyn is a redox sensor that mediates leukocyte wound attraction in vivo. Nature 2011; 480 (7375):109–12.
Sarraf KM, Belcher E, Raevsky E, Nicholson A, Goldstraw P, Lim E. Neutrophil/lymphocyte ratio and its association with survival after complete resection in non-small cell lung cancer. J. of Thorac. Cardiovasc. Surg. 2009; 137(2):425- 428.
Waugh DJ, Wilson C. The interleukin-8 pathway in cancer.Clin. Cancer Res. 2008; 14 (21):6735–41.
World Health Organization. Global TB Report 2015. Available from https://www.who.int › teams › tb-reports. Accessed 10th July, 2021.
Tamhane UU, Aneja S, Montgomery D, Rogers E.K, Eagle KA, Gurm HS. Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute coronary syndrome. Am. J. Card. 2008; 102:653–657.
de Jager CP, van Wijk PT, Mathoera RB, de JonghLeuvenink J, van der Poll V, Wever PC. Lymphocytopenia and neutrophil-lymphocyte count ratio predict bacteremia better than conventional infection markers in an emergency care unit. Crit Care 2010; 14:R192.
Goodman DA, Goodman CB, Monk JS. Use of the neutrophil:lymphocyte ratio in the diagnosis of appendicitis. Am Surg. 2012; 61:257–259.
Wu Q, Hu T, Zheng E, Deng X, Wang Z. Prognostic role of the lymphocyte-to-monocyte ratio in colorectal cancer. Medicine (Baltimore). 2017; 96(22): e7051.
Goto W, Kashiwagi S, Asano Y, Takada K, Takahashi K, Hatano T. Predictive value of lymphocyte-to-monocyte ratio in the preoperative setting for progression of patients with breast cancer. BMC Cancer 2018; 18:1137.
Akpan P, Akpotuzor J, Osim E. Haemostasis and Inflammation Cross-Talk in Tuberculosis Disease. Int. J. Lab. Hematol. 2019; 41:8.
Akwiwu EC, Alfred UO, Akpotuzor JO, Onukak, EE. Antenatal Care Coverage and the Prevalence of Syphilis, Viral Hepatitis and Human Immuno-Deficiency Virus Infections Among Pregnant Women in Uyo, Nigeria. J. Med. Lab. Sci. 2021; 31(3):11-19.
Ogbo FA, Ogeleka P, Okoro A, Olusanya BO, Olusanya J, Ifegwu IK. Tuberculosis disease burden and attributable risk factors in Nigeria, 1990-2016. Trop Med Health 2018; 46:34.
Akwiwu EC, Okafor AO, Akpan PA, Akpotuzor JO, Asemota EA, Okoroiwu HU, Anyanwu SO. P53 Protein Level and Some Haematologic Parameters among Women of Reproductive Age Living with HIV Infection. Niger. J. Physiol. Sci. 2021; 36: 85 – 89.
Mouabbi J, Zein R, Susanna S, Saravolatz L Kafri Z, Hadid T. Neutrophil-to-Lymphocyte Ratio and Platelet-toLymphocyte Ratio as Predictive markers for DVT. Chest Annual Meeting 2017; 152(4):A1041. 22. Abunimye DA, Akwiwu EC, Anyanwu SO, Onukak EE, Akpotuzor JO. Selected Inflammatory and Thrombotic Indicators among persons living with HIV infection in Southern Nigeria. Afr. J. Lab. Haematol. Transf. Sci. 2022;
(2):173-179.
Yang J, Zhang L, Yu HC, Yang X, Wang H. Monocyte and macrophage differentiation; circulation inflammatory marker monocyte as biomarker for inflammatory diseases. Biomark. Res. 2014; 2: 1.
Udosen, JE, Akwiwu EC, Akpotuzor DU, Akpotuzor JO. Blood Cell Count Ratios in Post-Operative Breast Cancer Patients on Chemotherapy. Afr. J. Lab. Haematol. Transf. Sci. 2022; 1(1):70-76.
Akwiwu EC, Ukpabi SA, Akpotuzor JO. Utility of Blood Cell Count Ratios as Biomarkers of Venous Thromboembolism Among Women on Oral Contraceptives. J. Med. Lab. Sci. 2022; 32 (1): 34-40.
Kroon EE, Coussens AK, Kinnear C, Orlova M, Möller M, Seeger A. Neutrophils: innate effectors of TB resistance? Front. Immunol. 2018; 9:2637.
Marshall JS, Warrington R, Watson W, Kim HL. An introduction to immunology and immunopathology. Allergy Asthma Clin. Immunol. 2018; 14:49.
Ndem BN, Akwiwu EC, Akpan PA, Akpotuzor JO, Bassey IE, Isong IK, Onukak EE. Timely accessing of antenatal care and prevalence of vitamin B12 and Folate deficiencies among pregnant women in a Nigerian population. New Zealand J. Medical Lab. Sci. 2021; 75: 12-15.