Protective Effect of Omega-3 and the Potential of Toll-like Receptor Gene Expression in Rats with Doxorubicin-induced Cardiac Toxicity http://.www.doi.org/10.26538/tjnpr/v7i2.9
Main Article Content
Abstract
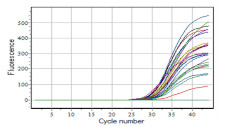
Despite the clinical signs of doxorubicin (DOX)-induced cardiomyopathy, the mechanisms underlying DOX-induced cardiac damage are unknown. Toll-like receptors (TLRs) allow cardiomyocytes to respond to either endogenous or external signals, both of which have the potential to alter the pathophysiological responses to dilated cardiomyopathy. Omega-3 (OMG-3) precursors are highly active metabolites with numerous therapeutic benefits in the prevention and/or treatment of a variety of diseases. Thus, this study was aimed at evaluating the preventive effect of omega-3 on rats suffering from acute DOX-induced cardiotoxicity associated with TLR gene expression. Thirty rats were divided into five equal groups; Group 1 received no treatment, Group 2 received doxorubicin (at a toxic dose of 20 mg/kg), and Groups 3-5 received doxorubicin (20 mg/kg) after receiving OMG-3 at various doses (100, 200, and 400 mg/kg/day, respectively) for 4 weeks. At the end of the experiment, blood samples were obtained from the heart. The real time polymerase chain reaction (RT-PCR) was used to assess TLR2 and TLR4 gene expression. TLR2 had a significantly (p<0.01) elevated fold change in the DOX alone group (28.74+4.95), whereas TLR2 expression was significantly reduced in the OMG-3 pretreated groups (1.633+0.51, 0.733+0.13, and 0.709+0.16, respectively). TLR4 fold change in the DOX alone group was 8.57+1.22, whereas TLR4 expression was significantly reduced in the OMG-3 pretreated groups (100, 200, and 400 mg/kg) with values of 0.809+0.32, 0.852+0.50, and 0.272+0.16, respectively. The findings of this study revealed that OMG-3 decreased doxorubicin-induced cardiotoxicity and showed a significant cardioprotective effect by lowering TLR2 and TLR4 gene expression.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
Kaklamani VG, Gradishar WJ. Epirubicin versus doxorubicin: which is the anthracycline of choice for the treatment of breast cancer? Clin Breast Canc. 2003; 4:S26-S33.
Cortés-Funes H, Coronado C. Role of anthracyclines in the era of targeted therapy. Cardiovasc Toxicol. 2007; 7(2):56-60.
Yagmurca M, Fadillioglu E, Erdoğan H, Ucar M, Sogut S,Irmak M. Erdosteine prevents doxorubicin-induced cardiotoxicity in rats. Pharmacol Res. 2003; 48:377-82.
Minotti G, Mancuso C, Frustaci A, Mordente A, Santini SA, Calafiore AM, et al. Paradoxical inhibition of cardiac lipid peroxidation in cancer patients treated with doxorubicin. Pharmacologic and molecular reappraisal of anthracycline cardiotoxicity. J Clin Invest. 1996; 98(3):650-61.
Venditti P, Balestrieri M, De Leo T, Di Meo S. Free radical involvement in doxorubicin-induced electrophysiological alterations in rat papillary muscle fibres. Cardiovasc Res. 1998; 38(3):695-702.
Zhou S, Palmeira CM, Wallace KB. Doxorubicin-induced persistent oxidative stress to cardiac myocytes. Toxicol Lett. 2001; 121(3):151-7.
Bruynzeel AM, Abou El Hassan MA, Schalkwijk C, Berkhof J, Bast A, Niessen HW, van der Vijgh WJ (2007). Antiinflammatory agents and mono HER protect against DOXinduced cardiotoxicity and accumulation of CML in mice. Brit J Canc. 2012; 96(6):937–943.
Morand EF. New therapeutic target in inflammatory disease: macrophage migration inhibitory factor. Intern Med J. 2005; 35(7):419-26.
Zernecke A, Bernhagen J, Weber C. Macrophage migration inhibitory factor in cardiovascular disease. Circul. 2008; 117(12):1594-602.
Uzun M, Kayaoğlu S, Ata P, Tilki M, Ocak S, Doğan T. Association of macrophage migration inhibitory factor gene-173 G/C polymorphism with occurrence and severity of acute pancreatitis. 2020;60(2):182–187.
He XX, Yang J, Ding YW, Liu W, Shen QY, Xia HH. Increased epithelial and serum expression of macrophage migration inhibitory factor (MIF) in gastric cancer: potential role of MIF in gastric carcinogenesis. Gut. 2006; 55(6):797-802.
De Angelis A, Piegari E, Cappetta D, Russo R, Esposito G, Ciuffreda LP, Ferraiolo FA, Frati C, Fagnoni F, Berrino L, Quaini F, Rossi F, Urbanek K. SIRT1 activation rescues doxorubicin-induced loss of functional competence of human cardiac progenitor cells. Int J Cardiol. 2015; 189:30-44.
Miyauchi S, Hirasawa A, Iga T, Liu N, Itsubo C, Sadakane K, Hara T, Tsujimoto G. Distribution and regulation of protein expression of the free fatty acid receptor GPR120. Naunyn Schmiedebergs Arch Pharmacol. 2009; 379(4):427-34.
Li AH, Liu PP, Villarreal FJ, García RA. Dynamic changes in myocardial matrix and relevance to disease: Translational perspectives. Circul Res. 2014; 114:916–27.
Cappetta D, Esposito G, Piegari E, Russo R, Ciuffreda LP, Rivellino A, Berrino L, Rossi F, De Angelis A, Urbanek K. SIRT1 activation attenuates diastolic dysfunction by reducing cardiac fibrosis in a model of anthracycline cardiomyopathy. Int J Cardiol. 2016; 205:99-110.
Venditti P, Balestrieri M, De Leo T, Di Meo S. Free radical involvement in doxorubicin-induced electrophysiological alterations in rat papillary muscle fibers. Cardiovasc Res. 1998; 38(3):695-702.
Zhou S, Palmeira CM, Wallace KB. Doxorubicin-induced persistent oxidative stress to cardiac myocytes. Toxicol Lett. 2001; 121(3):151-7.
Han C, Xu J, Liu CH, Li X, Zhai P, Hashan A, Song M. Modulation of TLR2 and TLR4 in macrophages following Trichinella spiralis infection. Helminthologia. 2018; 55(3):195-203.
Levy RJ, Piel DA, Acton PD, Zhou R, Ferrari VA, Karp JS, Deutschman CS. Evidence of myocardial hibernation in the septic heart. Crit Care Med. 2005 Dec;33(12):2752-6.
Pop-Moldovan AL, Trofenciuc NM, Dărăbanţiu DA, Precup C, Branea H, Christodorescu R, et al. Customized laboratory TLR4 and TLR2 detection method from peripheral human blood for early detection of doxorubicin-induced cardiotoxicity. Canc Gene Ther. 2017; 24(5):203-7.
Ahmed H, Khan MA, Kahlert UD, Niemelä M, Hänggi D, Chaudhry SR, Muhammad S. Role of adaptor protein myeloid differentiation 88 (MyD88) in post-subarachnoid hemorrhage inflammation: A systematic review. Int J Mol Sci. 2021; 22(8):4185.
Kigerl KA, de Rivero Vaccari JP, Dietrich WD, Popovich PG, Keane RW. Pattern recognition receptors and central nervous system repair. Exp Neurol. 2014; 258:5-16.
Yu L, Feng Z. The Role of Toll-like receptor signaling in the progression of heart failure. Mediators Inflamm. 2018; 9874109.
Chatterjee K, Zhang J, Honbo N, Karliner JS. Doxorubicin cardiomyopathy. Cardiol. 2010; 115(2):155-62.
Frantz S, Kelly RA, Bourcier T. Role of TLR-2 in the activation of nuclear factor kappa B by oxidative stress in cardiac myocytes. J Biol Chem. 2001; 276(7):5197-203.
Guo J, Friedman SL. Toll-like receptor 4 signaling in liver injury and hepatic fibrogenesis. Fibrogenesis Tiss Rep. 2010; 3:21.
Katare PB, Bagul PK, Dinda AK, Banerjee SK. Toll-Like Receptor 4 inhibition improves oxidative stress and mitochondrial health in isoproterenol-induced cardiac hypertrophy in rats. Front Immunol. 2017; 8:719.
Nozaki N, Shishido T, Takeishi Y, Kubota I. Modulation of doxorubicin-induced cardiac dysfunction in Toll-like receptor-2– knockout mice. Circul. 2004; 110(18):2869-74.
Zhang YJ, Huang H, Liu Y, Kong B, Wang G. MD-1 deficiency accelerates myocardial inflammation and apoptosis in doxorubicin-induced cardiotoxicity by activating the TLR4/MAPKs/nuclear factor kappa B (NF-κB) signaling pathway. Med Sci Monit. 2019; 25:7898-907.