Effects of Saffron (Crocus sativus L) Compared to Atorvastatin on the Livers of Hypercholesterolemia Rat Models
Main Article Content
Abstract
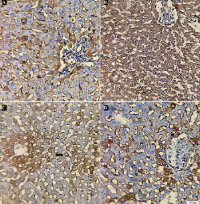
Hypercholesterolemia is characterized by elevated blood total cholesterol, and might induce liver inflammation. Atorvastatin as the first-line medication in hypercholesterolemia can cause side effects; Saffron has been reported to have hepatoprotective property. This study compared the anti-inflammatory and hepatoprotective effects of Saffron vs. Atorvastatin on the liver of high-fat diet-induced hypercholesterolemia male rats. Thirty-two rats were divided equally into four groups and given a high-fat diet (36 days). The third group was given Saffron (80 mg/kg of body weight/day), and the fourth group was given Atorvastatin (0.2 mg/200 g of body weight/day) from days 16-36. Data were analyzed using SPSS 24.0 with a significance level of p<0.05. Total cholesterol (TC) between groups was significantly different at day 15 (p<0.01), while at day 37, the Atorvastatin group had a closer TC to the normal diet group than the Saffron group. Expression of Tumor Necrosis Factor-alpha (TNF-α) in the high-fat diet group (p<0.01) was significantly higher than that in the Saffron group (p<0.01), Atorvastatin group (p<0.01) as well as the control (p<0.01). The values of total hepatocyte degeneration, the number of inflammatory foci, and the total area width of inflammatory foci in the high-fat diet group were significantly higher than those in the Saffron group (p<0.01, p<0.01, p<0.01, respectively), than those in the Atorvastatin group (p<0.01, p<0.01, p<0.01, respectively) than in the control group (p<0.01, p<0.01, p<0.01, respectively). Saffron exhibited drug-likeness potential as a natural hepatoprotective agent. Further research is needed to understand better the mechanisms underlying Saffron's protective effects.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
1. Berta E, Zsíros N, Bodor M, Balogh I, Lőrincz H, Paragh G, Harangi M. Clinical aspects of genetic and non-genetic cardiovascular risk factors in familial hypercholesterolemia. Genes. 2022; 13(7):1158. Doi: 10.3390/genes13071158
2. González-Lleó AM, Sánchez-Hernández RM, Boronat M, Wägner AM. Diabetes and familial hypercholesterolemia: interplay between lipid and glucose metabolism. Nutrients. 2022; 14(7):1503. Doi: 10.3390/nu14071503
3. Lesmana R, Tandi YYP, Megantara I, Rosdianto AM, Goenawan H, Christoper A, Gunadi JW, Radhiyanti PT, Zulhendri F. Propolis extract alters the abundance of bacteroides thetaiotaomicron and faecalibacterium prausnitzii, and ileum mucosal structure of male wistar rats with high-fat diet. Trop J Nat Prod Res. 2024; 8(7):7650–7657. Doi: 10.26538/tjnpr/v8i7.4
4. Morofuji Y, Nakagawa S, Ujifuku K, Fujimoto T, Otsuka K, Niwa M, Tsutsumi K. Beyond lipid-lowering: effects of statins on cardiovascular and cerebrovascular diseases and cancer. Pharmaceuticals. 2022; 15(2):151. Doi: 10.3390/ph15020151
5. Ray S. Role of statins in the management of dyslipidaemia. Indian Heart J. 2024; 76:S33–S37. Doi: 10.1016/j.ihj.2023.11.267
6. Rugivarodom M, Geeratragool T, Pausawasdi N, Charatcharoenwitthaya P. Fatty pancreas: linking pancreas pathophysiology to nonalcoholic fatty liver disease. J Clin Transl Hepatol. 2022; 10(6):1229–39. Doi: 10.14218/JCTH.2022.00085
7. Noreen S, Rehman H, Tufail T, Ain HBUI, Awuchi CG. Secoisolariciresinol diglucoside and anethole ameliorate lipid abnormalities, oxidative injury, hypercholesterolemia, heart, and liver conditions. Food Sci Nut. 2023; 11(6):2620–2630. Doi: 10.1002/fsn3.3250
8. Galimberti F, Casula M, Olmastroni E. Apolipoprotein B compared with low-density lipoprotein cholesterol in the atherosclerotic cardiovascular diseases risk assessment. Pharmacol Res. 2023; 195:106873. Doi: 10.1016/j.phrs.2023.106873
9. Lee ZV, Llanes EJ, Sukmawan R, Thongtang N, Ho HQT, Barter P. Prevalence of plasma lipid disorders with an emphasis on LDL cholesterol in selected countries in the Asia-Pacific region. Lipids Health Dis. 2021; 20(1):33. Doi: 10.1186/s12944-021-01450-8
10. Nudhar L, Subandrate S, Susilawati S, Oswari L. Mean differences of total cholesterol levels among vegetarians and non-vegetarians at Maha Vihara Maitreya Duta Palembang, Indonesia. Fol Med Indones. 2020; 56(3):197. Doi: 10.20473/fmi.v56i3.24555
11. Handelsman Y, Jellinger PS, Guerin CK, Bloomgarden ZT, Brinton EA, Budoff MJ, Davidzon MH, Einhorn D, Fazio S, Fonseca VA, Garber AJ, Grunberger G, Krauss RM, Mechanick JI, Rosenblit PD, Smith DA, Wyne KL. Consensus statement by the american association of clinical endocrinologists and american college of endocrinology on the management of dyslipidemia and prevention of cardiovascular disease algorithm-2020 executive summary. Endocr Pract. 2020; 26(10):1196–1224. Doi: 10.4158/CS-2020-0490
12. Kalanjati VP, Oktariza RT, Suwito BE, Pradana KA, Rahmawan D, Abdurachman A. Cardiovascular disease risk factors and anthropometry features among seemingly healthy young adults. Int J Public Health Sci. 2021; 10(1):77–82. Doi: 10.11591/ijphs.v10i1.20554
13. Isdadiyanto S, Pratiwi AR, Mardiati SM. Liver histopathology of rats induced by high-fat feed after giving neem leaf ethanol extract. J Bio Bio Edu. 2022; 14(2):254-262. Doi:10.15294/biosaintifika.v14i2.34383
14. Rashwan AG, Assar DH, Salah AS, Liu X, Al-Hawary II, Abu-Alghayth MH, Salem SMR, Khalil K, Hanafy NAN, Abdelatty A, Sun L, Elbialy ZI. Dietary chitosan attenuates high-fat diet-induced oxidative stress, apoptosis, and inflammation in nile tilapia (oreochromis niloticus) through regulation of nrf2/kaep1 and bcl-2/bax pathways. Biology. 2024; 13(7):486. Doi: 10.3390/biology13070486
15. Aziz MA, Rejeki PS, I’tishom R, Yuliawati TH. Effect of heated canola oil on aorta wall thickness in rats. MBIOMJ. 2022; 32(2):82–88. Doi: 10.20473/mbiom.v32i2.2022.82-88
16. Ibrahim MA, Asuka E, Jialal I. Hypercholesterolemia. In: StatPearls [Internet]. StatPearls Publishing. 2023 [cited 2024 Sept 5]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459188/
17. Ruscica M, Ferri N, Banach M, Sirtori CR, Corsini A. Side effects of statins: from pathophysiology and epidemiology to diagnostic and therapeutic implications. Cardiovasc Res. 2022; 118(17):3288–3304. Doi: 10.1093/cvr/cvac020
18. Cheon DY, Jo SH. Adverse effects of statin therapy and their treatment. Cardiovasc Prev Pharmachoter. 2022; 4(1):1–6. Doi: 10.36011/cpp.2022.4.e4
19. Osawa Y, Hoshi M, Yasuda I, Saibara T, Moriwaki H, Kozawa O. Tumor necrosis factor-α promotes cholestasis-induced liver fibrosis in the mouse through tissue inhibitor of metalloproteinase-1 production in hepatic stellate cells. PloS One. 2013; 8(6):e65251. Doi: journal.pone.0065251
20. Hasan NA, Kalanjati VP, Purwantari KE, Abdurachman A, Miftahussurur M. Atorvastatin versus tetrahydrolipstatin in male patients with dyslipidemia: a systematic review and meta-analysis. J Pharm Pharmacogn Res. 2024; 12(2):218–230. Doi: 10.56499/jppres23.1741_12.2.218
21. Filppula AM, Hirvensalo P, Parviainen H, Ivaska VE, Lönnberg KI, Deng F, Viinamaki J, Kurkela M, Neuvonen M, Niemi M. Comparative hepatic and intestinal metabolism and pharmacodynamics of statins. Drug Metab Dispos. 2021; 49(8):658–667. Doi: 10.1124/dmd.121.000406
22. Schonewille M, Boer JF, Mele L, Wolters H, Bloks VW, Wolters JC, Kuivenhoven JA, Tietge UJF, Brufau G, Groen AK. Statins increase hepatic cholesterol synthesis and stimulate fecal cholesterol elimination in mice. J Lipid Res. 2016; 57(8):1455–1464. Doi: 10.1194/jlr.M067488
23. Butnariu M, Quispe C, Herrera-Bravo J, Sharifi-Rad J, Singh L, Aborehab NM, Bouyahya A, Venditti A, Sen S, Acharya K, Bashiry M, Ezzat SM, Setzer WN, Martorell M, Mileski KS, Bagiu LC, Docea AO, Calina D, Cho WC. The pharmacological activities of crocus sativus l.: a review based on the mechanisms and therapeutic opportunities of its phytoconstituents. Oxid Med Cell Longev. 2022; 2022:8214821. Doi: 10.1155/2022/8214821
24. Mir RA, Tyagi A, Hussain SJ, Almalki MA, Zeyad MT, Deshmukh R, Ali S. Saffron, a potential bridge between nutrition and disease therapeutics: global health challenges and therapeutic opportunities. Plants. 2024; 13(11):1467. Doi: 10.3390/plants13111467
25. El Midaoui A, Ghzaiel I, Vervandier-Fasseur D, Ksila M, Zarrouk A, Nury T, Khallouki F, El Hessni A, Ibrahimi SO, Latruffe N, Couture R, Kharoubi O, Brahmi F, Hammami S, Kouki OM, Hammami M, Ghrairi T, Vejux A, Lizard G. Saffron (crocus sativus l.): a source of nutrients for health and for the treatment of neuropsychiatric and age-related diseases. Nutrients. 2022; 14(3):597. Doi: 10.3390/nu14030597
26. Sabirosi BG. Ekspresi tumor necrosis factor – alpha (tnf - α) dan jumlah sperma pada tikus (rattus norvegicus) model diabetes melitus tipe 1 hasil induksi streptozotocin yang diterapi dengan ekstrak etanol rimpang. Dis Universitas Brawijaya. 2014. https://repository.ub.ac.id/id/eprint/126924/
27. Bai Y, Chen K, Liu J, Wang Y, Wang C, Ju S, Zhou C, Yao W, Xiong B, Zheng C. Activation of AMPK pathway by low‑dose donafenib and atorvastatin combination improves high‑fat diet‑induced metabolic dysfunction‑associated steatotic liver disease. Mol Med Rep. 2024; 29(3):51. Doi: 10.3892/mmr.2024.13175
28. Gradel AKJ, Holm SK, Byberg S, Merkestein M, Hogendorf WFJ, Lund ML, Buijink JA, Damgaard J, Lykkesfeldt J, Holst B. The dietary regulation of LEAP2 depends on meal composition in mice. Faseb J. 2023; 37(6):e22923. Doi: 10.1096/fj.202201828R
29. Hoshyar R, Hosseinian M, Naghandar MR, Hemmati M, Zarban A, Amini Z, Valavi M, Beyki MZ, Mehrpour O. Anti-dyslipidemic properties of saffron: reduction in the associated risks of atherosclerosis and insulin resistance. Iran Red Crescent Med J. 2016; 18(12):e36226. Doi: 10.5812/ircmj.36226
30. Nair AB, Jacob S. A simple practice guide for dose conversion between animals and human. J Basic Clin Pharm. 2016; 7(2):27–31. Doi: 10.4103/0976-0105.177703
31. Rejeki PS, Putri EAC, Prasetya RE. Ovariektomi pada tikus dan mencit. Surabaya: Airlangga University Press. 2019. https://repository.unair.ac.id/94079/
32. John LM, Petersen N, Gerstenberg MK, Torz L, Pedersen K, Christoffersen BØ, Kuhre RE. Housing-temperature reveals energy intake counter-balances energy expenditure in normal-weight, but not diet-induced obese, male mice. Commun Biol. 2022; 5(1):946. Doi: 10.1038/s42003-022-03895-8
33. Boudjeko T, Ngomoyogoli JEK, Woguia AL, Yanou NN. Partial characterization, antioxidative properties and hypolipidemic effects of oilseed cake of allanblackia floribunda and jatropha curcas. BMC Complement Altern Med. 2013; 13:352. Doi: 10.1186/1472-6882-13-352
34. Abd Rahim IN, Mohd Kasim NA, Isa MR, Nawawi H. A systematic review on the effect of saffron extract on lipid profile in hyperlipidaemic experimental animal models. Malays J Med Sci. 2022; 29(4):14–27. Doi: 10.21315/mjms2022.29.4.3
35. Hickman DL, Swan M. Use of a body condition score technique to assess health status in a rat model of polycystic kidney disease. J Am Assoc Lab Anim Sci. 2010; 49(2):155–159. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2846001/
36. Arora JS, Kim JK, Pakvasa M, Sayadi LR, Lem M, Widgerow AD, Leis AR. Microsurgical needle retention does not cause pain or neurovascular injury in a rat model. Plast Reconstr Surg Glob Open. 2023; 11(8):e5171. Doi: 10.1097/GOX.0000000000005171
37. Weber B, Lackner I, Haffner-Luntzer M, Palmer A, Pressmar J, Scharffetter-Kochanek K, Knöll B, Schrezenemeier H, Relja B, Kalbitz M. Modeling trauma in rats: similarities to humans and potential pitfalls to consider. J Transl Med. 2019; 17(1):305. Doi: 10.1186/s12967-019-2052-7
38. Patil V, Hardikar H, Joshi S, Tembe S. Optical detection of total cholesterol based on a dye-displacement method. Spectrochim Acta A Mol Biomol Spectrosc. 2023; 293:122425. Doi: 10.1016/j.saa.2023.122425
39. Romano E, Cataldo PG, Iramain MA, Castillo MV, Manzur ME, Antonia Brandán SA. Identification of cholesterol in different media by using the FT-IR, FT-Raman and UV–visible spectra combined with DFT calculations. J Mol Liquids. 2024; 403:124879. Doi: 10.1016/j.molliq.2024.124879
40. Felgendreff P, Schindler C, Mussbach F, Xie C, Gremse F, Settmacher U, Dahmen U. Identification of tissue sections from decellularized liver scaffolds for repopulation experiments. Heliyon. 2021; 7(2):e06129. Doi: 10.1016/j.heliyon.2021.e06129
41. Koivukoski S, Khan U, Ruusuvuori P, Latonen L. Unstained tissue imaging and virtual hematoxylin and eosin staining of histologic whole slide images. Lab Invest. 2023; 103(5):100070. Doi: 10.1016/j.labinv.2023.100070
42. Zhang P, Shen H, Huang J, Wang H, Zhang B, Zhou R, Zhong B, Fan X. Intraperitoneal administration of fetuin-a attenuates d-galactosamine/lipopolysaccharide-induced liver failure in mouse. Dig Dis Sci. 2014; 59(8):1789–1797. Doi: 10.1007/s10620-014-3071-0
43. Mashmoul M, Azlan A, Mohtarrudin N, Mohd Yusof BN, Khaza’ai H, Khoo HE, Farzadnia M, Boroushaki MT. Protective effects of saffron extract and crocin supplementation on fatty liver tissue of high-fat diet-induced obese rats. BMC Complement Altern Med. 2016; 16(1):401. Doi: 10.1186/s12906-016-1381-9
44. Ayyed MF, Hussein FF, Mohammed MJ. Physiological effects of some medicinal plants on the development of non-alcoholic fatty liver disease in male laboratory rats. IOP Conf Ser: Earth Environ Sci. 2024; 1371(6):062022. Doi: 10.1088/1755-1315/1371/6/062022
45. Ali FAZ, Abdel-Maksoud FM, Abd Elaziz HO, Al-Brakati A, Elmahallawy EK. Descriptive histopathological and ultrastructural study of hepatocellular alterations induced by aflatoxin B1 in rats. Animals. 2021; 11(2):509. Doi: 10.3390/ani11020509
46. Schneider CA, Rasband WS, Eliceiri KW. NIH Image to ImageJ: 25 years of image analysis. Nat Methods. 2012; 9(7):671–675. Doi: 10.1038/nmeth.2089
47. Yalçın T, Kaya S, Tektemur NK, Ozan İE. The methods used in histopathological evaluation of testis tissues. Batman univ yaşam bilim derg. 2020; 10(1):148–157. https://dergipark.org.tr/en/pub/buyasambid/issue/55551/617431
48. Kalanjati VP, Hendrata MW, Ardana FN. Cellular composition in the aging cerebral cortex of humans. Neurophysiology. 2019; 51(6):424–429. Doi: 10.1007/s11062-020-09838-5
49. Gouda MA. Common pitfalls in reporting the use of SPSS software. Med Princ Pract. 2015; 24(3):300. Doi: 10.1159/000381953
50. IBM Corp. IBM SPSS statistics for windows, version 24.0. Armonk, NY: IBM Corp. 2024. https://www.ibm.com/spss
51. Mala FA. Basic statistics and epidemiology: a practical guide (5th edition). Technometrics. 2022; 64(4):578–579. Doi: 10.1080/00401706.2022.2126657
52. Gradel AKJ, Holm SK, Byberg S, Merkestein M, Hogendorf WFJ, Lund ML, Buijink JA, Dambgaard J, Lykkesfeldt J, Holst B. The dietary regulation of LEAP2 depends on meal composition in mice. Faseb J. 2023; 37(6):e22923. Doi: 10.1096/fj.202201828R
53. Yoon H, Lee Y, Park H, Kang HJ, Ji Y, Holzapfel WH. Lactobacillus johnsonii BFE6154 ameliorates diet-induced hypercholesterolemia. Probiotics & Antimicro Prot. 2023; 15(3):451–459. Doi: 10.1007/s12602-021-09859-4
54. González-Mañán D, D’Espessailles A, Dossi CG, San Martín M, Mancilla RA, Tapia GS. Rosa mosqueta oil prevents oxidative stress and inflammation through the upregulation of PPAR-α and NRF2 in C57BL/6J mice fed a high-fat diet1. J Nutr. 2017; 147(4):579–588. Doi: 10.3945/jn.116.243261
55. Alipour R, Aryaeian N, Hajiluian G, Soleimani M, Barati M. The effect of the saffron intervention on NAFLD status and related gene expression in a rat model. Med J Islam Repub Iran. 2023; 37:28. Doi: 10.47176/mjiri.37.28
56. Çeter T, Mollaamin F, Monajjemi M. A Comprehensive overview of the effects of saffron extract and its ingredients on neurologic, diabetes, cardiovascular and gastrointestinal diseases: biological studies using CRISPR-Cas9, Docking, Omics and Bioinformatics Approaches. J Biol Reg and Homeo Agents. 2023; 37(8):3955–3976. Doi: 10.23812/j.biol.regul.homeost.agents.20233708.391
57. Jiang H, Huang X, Wang J, Zhou Y, Ren C, Zhou T, Pei J. Hepatoprotective effect of medicine food homology flower saffron against CCl4-induced liver fibrosis in mice via the Akt/HIF-1α/VEGF signaling pathway. Molecules. 2023; 28(21):7238. Doi: 10.3390/molecules28217238
58. Samarghandian S, Azimi-Nezhad M, Samini F. Ameliorative effect of saffron aqueous extract on hyperglycemia, hyperlipidemia, and oxidative stress on diabetic encephalopathy in streptozotocin induced experimental diabetes mellitus. BioMed Res Int. 2014; 2014(1):920857. Doi: 10.1155/2014/920857
59. Elgazar AF, Rezq AA, Bukhari HM. Anti-hyperglycemic effect of saffron extract in alloxan-induced diabetic rats. Europ J Biol Sci. 2013; 5(1):14-22. Doi: 10.5829/idosi.ejbs.2013.5.1.7224
60. Khan TJ, Ahmed YM, Zamzami MA, Mohamed SA, Khan I, Baothman OAS, Mehanna MG, Yasir M. Effect of atorvastatin on the gut microbiota of high fat diet-induced
61. hypercholesterolemic rats. Sci Rep. 2018; 8(1):662. Doi:10.1038/s41598-017-19013-2
62. Ji G, Zhao X, Leng L, Liu P, Jiang Z. Comparison of dietary control and atorvastatin on high fat diet induced hepatic steatosis and hyperlipidemia in rats. Lipids Health Dis. 2011; 10:23. Doi: 10.1186/1476-511X-10-23
63. Mclver LA, Siddique MS. Atorvastatin. In: StatPearls [Internet]. StatPearls Publishing. 2020 [cited 2024 Sept 6]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430779/
64. Feng L, Huang F, Ma Y, Tang J. The effect of high-fat diet and exercise intervention on the TNF-α level in rat spleen. Front Immunol. 2021; 12:671167. Doi: 10.3389/fimmu.2021.671167
65. Lee EJ, Edward OC, Seo EB, Mun EG, Jeong SJ, Ha G, Han A, Cha YS. Gochujang ameliorates hepatic inflammation by improving dysbiosis of gut microbiota in high-fat diet-induced obese mice. Microorganisms. 2023; 11(4):911. Doi: 10.3390/microorganisms11040911
66. Syarif, Rasyid H, Aman M, Lawrence GS, Bukhari A, Patellongi I, Cangara H, Putra MZDA. The effects of high fat diet on the incidence of obesity and monocyte chemoattractant protein-1 levels on histological changes in prostate wistar rats. Res Rep Urol. 2024; 16:57–63. Doi: 10.2147/RRU.S437322
67. Ashrafi M, Afsar Z, Erjaee H, Nazifi S. The effects of saffron (crocus sativus) aqueous extract on TNF-α levels in liver, kidney, and lens tissues of diabetic rats. Turk J Endocrinol Metab. 2018; 22:217–224. Doi: 10.25179/tjem.2018-59710
68. Melasari WP, Suharjono S, Samsulhadi W. Effect of atorvastatin in lipid profile changes and inflammation marker TNF-alpha on diabetes patient with dyslipidemia. Fol Med Indones. 2021; 57(1):6–10. Doi: 10.20473/fmi.v57i1.26326
69. Eldesoqui M, Mohamed AS, Nasr ANA, Ali SK, Eldaly MM, Embaby EM, Ahmed HS, Saeed ZM, Mohammed ZA, Soliman RHM. The renoprotective effect of atorvastatin in a rat model of high-fat high-fructose diet-induced renal injury. Egypt Acad J Biolog Sci (D-Histology and Histochemistry). 2024; 16(1):179–194. Doi: 10.21608/eajbsd.2024.360842
70. Maqbool Z, Arshad MS, Ali A, Aziz A, Khalid W, Afzal MF, Bangar SP, Addi M, Hano C, Lorenzo JM. Potential role of phytochemical extract from saffron in development of functional foods and protection of brain-related disorders. Oxid Med Cell Longev. 2022; 2022(1):6480590. Doi: 10.1155/2022/6480590
71. Elfardi YR, El Boukhari R, Fatimi A, Bouissane L. The multifaceted therapeutic potential of saffron: an overview based on research and patents. Drugs and Drug Candidates. 2024; 3(3):437–454. Doi: 10.3390/ddc3030026
72. Rahim INA, Kasim NAM, Omar E, Muid SA, Nawawi H. Safety evaluation of saffron extracts in early and established atherosclerotic New Zealand white rabbits. PloS One. 2024; 19(1):e0295212. Doi: 10.1371/journal.pone.0295212
73. Inia JA, Stokman G, Pieterman EJ, Morrison MC, Menke AL, Verschuren L, Caspers MPM, Giera M, Jukema JW, Hoek AM, Princen MG. Atorvastatin attenuates diet-induced non-alcoholic steatohepatitis in apoe*3-leiden mice by reducing hepatic inflammation. Int J Mol Sc. 2023; 24(9):7818. Doi: 10.3390/ijms24097818
74. Lian CY, Zhai ZZ, Li ZF, Wang L. High fat diet-triggered non-alcoholic fatty liver disease: a review of proposed mechanisms. Chem Biol Interact. 2020; 330:109199. Doi: 10.1016/j.cbi.2020.109199
75. Radhakrishnan S, Yeung SF, Ke JY, Antunes MM, Pellizzon MA. Considerations when choosing high-fat, high-fructose, and high-cholesterol diets to induce experimental nonalcoholic fatty liver disease in laboratory animal models. Curr Dev Nutr. 2021; 5(12):nzab138. Doi: 10.1093/cdn/nzab138
76. Jeong HS, Kim KH, Lee IS, Park JY, Kim Y, Kim KS, Jang HJ. Ginkgolide a ameliorates non-alcoholic fatty liver diseases on high fat diet mice. Biomed Pharmacother. 2017; 88:625–634. Doi: 10.1016/j.biopha.2017.01.114
77. Tamada H, Naito H, Kitamori K, Hayashi Y, Yamagishi N, Kato M, Nakajima T. Efficacy of dietary lipid control in healing high-fat and high-cholesterol diet-induced fibrotic steatohepatitis in rats. PloS One. 2016; 11(1):e0145939. Doi: 10.1371/journal.pone.0145939