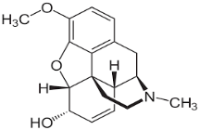
Evaluation of Oxidative Stress Levels in Codeine-Induced and Codeine Recovery Phase of Albino Rats
Main Article Content
Abstract
The widespread availability and potential for misuse of codeine have rendered chronic use a pressing public health issue. Long-term codeine exposure can lead to multisystem toxicity, causing oxidative stress, cellular damage, and increased vulnerability to illness. This study assessed the levels of oxidative stress in Albino rats during the codeine-induced and codeine-recovery phases. For this study, 20 Albino rats weighing 160-200 g were used. The animals were assigned into four groups of five rats. Feed and water were administered to rats in Group 1 (control). Codeine was administered to Groups 2, 3, and 4 at doses of 10 mg/kg, 15 mg/kg, and 20 mg/kg body weight, respectively. Serum biochemical assays were conducted using blood samples collected on day 14. After that, the animals underwent a 7-day codeine withdrawal to assess recovery. Blood samples were collected on day 7 for the second phase of biochemical assay. Administration of codeine for 14 days significantly reduced antioxidant enzyme levels (superoxide dismutase, glutathione reductase, catalase, and glutathione peroxidase) (p < 0.05), but serum lipid peroxidation level was elevated (p < 0.05). After a 7-day recovery period, catalase, glutathione reductase, and glutathione peroxidase levels showed significant recovery (p < 0.05), lipid peroxidation decreased significantly (p < 0.05), but superoxide dismutase levels remained unchanged. These findings indicate that misuse of codeine adversely affects oxidative stress levels, persisting even after recovery. Therefore, caution is recommended when consuming codeine and other opioids.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
Paltov Ye, Masna Z, Horbova N. Normal Indicators of Oxidative Stress and The Dynamics of Their Changes at Different Terms of Experimental Opioid Influence. Clin Anat and Oper Surg. 2022; 21(3), 22-28. doi: 10.24061/1727-0847.
Bronkhorst E, Adamjee M, Poka M. The misuse of codeine-containing medicines: Perceptions and behaviours of qualified pharmacy professionals. S Afr Fam Pract. 2024;10;66(1): e1-e7. doi: 10.4102/safp. v66i1.5862.
Kirschbaum M, Barnett T, Cross M. Experiences of over-the-counter codeine misusers and accounts of recovery: A qualitative study in Tasmania, Australia. Drug Alc Rev. 2020;39(7):879-887. doi: 10.1111/dar.13081.
Archibong VB, Usman IM, Lemuel AM. Prolonged Codeine Administration Causes Degeneration of Myelinated Axons and Motor Dysfunction in Wistar Rats. Subst Abuse Rehabil. 2022; 13:73-81. doi: 10.2147/SAR.S365982.
Thompson BL, Oscar-Berman M, Kaplan GB. Opioid-induced structural and functional plasticity of medium-spiny neurons in the nucleus accumbens. Neurosci Biobehav Rev. 2021; 120:417-430. doi: 10.1016/j.neubiorev.2020.10.015
Pizzino G, Irrera N, Cucinotta M, Pallio G, Mannino F, Arcoraci V, Squadrito F, Altavilla D, Bitto A. Oxidative Stress: Harms and Benefits for Human Health. Oxid Med Cell Longev. 2017; 2017:8416763. doi: 10.1155/2017/8416763.
Jomova K, Raptova R, Alomar SY, Alwasel SH, Nepovimova E, Kuca K, Valko M. Reactive oxygen species, toxicity, oxidative stress, and antioxidants: chronic diseases and ageing. Arch Toxicol. 2023; 97(10), 2499–2574. https://doi.org/10.1007/s00204-023-03562-9
Muscolo A, Mariateresa O, Giulio T, Mariateresa R. Oxidative Stress: The Role of Antioxidant Phytochemicals in the Prevention and Treatment of Diseases. Int. J. Mol. Sci. 2024; 25, 3264. https://doi.org/10.3390/ijms25063264
Singh A, Kukreti R, Saso L, Kukreti S. Oxidative Stress: A Key Modulator in Neurodegenerative Diseases. Mol. 2019;24(8):1583.
Murphy MP, Bayir H, Belousov V, Chang CJ, Davies KJA, Davies MJ, Dick TP, Finkel T, Forman HJ, Janssen-Heininger Y, Gems D, Kagan VE, Kalyanaraman B, Larsson NG, Milne GL, Nyström T, Poulsen HE, Radi R, Van Remmen H, Schumacker PT, Thornalley PJ, Toyokuni S, Winterbourn CC, Yin H, Halliwell B. Guidelines for measuring reactive oxygen species and oxidative damage in cells and in vivo. Nat Metab. 2022;4(6):651-662. doi:10.1038/s42255-022-00591-z
Dokunmu TM, Opara SC, Awani OU, Enoma DO, Adelani BI, Rotimi OA, Yakubu OF. Effects of Caffeine-Artemisinin Combination on Liver Function and Oxidative Stress in Selected Organs in 7,12- Dimethylbenzanthracene-Treated Rats. Trop J Nat Prod Res. 2021; 5(5):963-969. doi.org/10.26538/tjnpr/v5i5.27
Sriramcharan P, Jawahar N, Rajeshkumar R, Arivuselvam R, Antony J, Ganganagappa N, Venkatachalam S. Effects of Cerium Oxide and Selected Heavy Metals on the Induction of Cell Death Via Oxidative Stress-Mediated DNA Damage. Trop J Nat Prod Res. 2022; 6(7): 1108-1112.doi.org/10.26538/tjnpr/v6i7.11
Zahmatkesh M, Kadkhodaee M, Salarian A, Seifi B, Adeli S. Impact of opioids on oxidative status and related signalling pathways: An integrated view. J Opioid Manag. 2017;13(4):241-251. doi:10.5055/jom.2017.0392.
Mohammadnejad L, Soltaninejad K. Tramadol-induced organ toxicity via oxidative stress: a review study. International Journal of Medical Toxicology and Forensic Med. 2022;12(1):35430.
Sun Y, Oberley LW, Li Y. A simple method for clinical assay of superoxide dismutase. Clin Chem. 1988;34(3):497-500.
Aebi H. Catalase in vitro. Methods Enzymol. 1984; 105:121-126. doi:10.1016/s0076-6879(84)05016-3
Paglia DE, Valentine WN. Studies on the quantitative and qualitative characterisation of erythrocyte glutathione peroxidase. J Lab Clin Med. 1967;70(1):158-169.
Buege JA, Aust SD. Microsomal lipid peroxidation. Methods Enzymol. 1978; 52:302-310. doi:10.1016/s0076-6879(78)52032-6
Ajayi AF, Akhigbe RE. Codeine-induced sperm DNA damage is mediated predominantly by oxidative stress rather than apoptosis. Redox Rep. 2020;25(1):33-40. doi: 10.1080/13510002.2020.1752003.
Ogili F, Ali D, Attamah G, Aletan U, Nwani C. Morphometric, hematological and oxidative stress changes in Clarias gariepinus following sub-chronic exposure to tramadol. Com Bio and Phy Part C Tox & Pharm. 2021; 248(4):109096
Akhigbe R, Ajayi A. Testicular toxicity following chronic codeine administration is via oxidative DNA damage and up-regulation of NO/TNF-α and caspase 3 activities. PLoS One. 2020;15(3): e0224052. doi: 10.1371/journal.pone.0224052.
Younus H. Therapeutic potentials of superoxide dismutase. Int J Health Sci. (Qassim) 2018; 12(3):88-93
Dominko K, Dikic D, Hecimovic S. Enhanced activity of superoxide dismutase is a common response to dietary and genetically induced increased cholesterol levels. Nutr Neurosci. 2020;(5):398-410. doi: 10.1080/1028415X.2018.1511027
Jiang XY, Chen Q, Chen XY, Sun QY, Jing F, Zhang HQ, Xu J, Li XH, Guan QB. Superoxide dismutases: marker in predicting reduced left ventricular ejection fraction in patients with type 2 diabetes and acute coronary syndrome. BMC Cardiovasc Disord. 2024;24(1):191. doi: 10.1186/s12872-024-03867-2.
Nandi A, Yan LJ, Jana CK, Das N. Role of Catalase in Oxidative Stress- and Age-Associated Degenerative Diseases. Oxid Med Cell Longev. 2019; 2019:9613090. doi: 10.1155/2019/9613090.
Wróblewska J, Wróblewski M, Hołyńska-Iwan I, Modrzejewska M, Nuszkiewicz J, Wróblewska W, Woźniak A. The Role of Glutathione in Selected Viral Diseases. Antioxi. 2023; 12(7):1325. https://doi.org/10.3390/antiox12071325
Lin TH, Rao MY, Lu HW, Chiou CW, Lin ST, Chao HW, Zheng ZL, Cheng HC, Lee TM. A role for glutathione reductase and glutathione in the tolerance of Chlamydomonas reinhardtii to photo-oxidative stress. Physiol Plant. 2018;162(1):35-48. doi:10.1111/ppl.12622
Hong KS, Pagan K, Whalen W, Harris R, Yang J, Stout-Delgado H, Cho SJ. The Role of Glutathione Reductase in Influenza Infection. Am J Respir Cell Mol Biol. 2022;67(4):438-445. doi: 10.1165/rcmb.2021-0372OC.
Bao YJ, Zhou Q, Yu X, Yu X, Castellino FJ. Analysis and Characterisation of Glutathione Peroxidases in an Environmental Microbiome and Isolated Bacterial Microorganisms. J Microbiol Biotechnol. 2023;33(3):299-309. doi: 10.4014/jmb.2209.09006.
Handy DE, Loscalzo J. The role of glutathione peroxidase-1 in health and disease. Free Radic Biol Med. 2022; 188:146-161. doi: 10.1016/j.freeradbiomed.2022.06.004.
Chen PK, Yeo KJ, Huang PH, Chang SH, Chang CK, Lan JL, Chen DY. Increased Lipid Peroxidation May Be Linked to Ferritin Levels Elevation in Adult-Onset Still’s Disease. Biomed. 2021;9(11):1508. doi: 10.3390/biomedicines9111508.
Fu Y, He Y, Phan K, Bhatia S, Pickford R, Wu P, Dzamko N, Halliday GM, Kim WS. Increased unsaturated lipids underlie lipid peroxidation in synucleinopathy brain. Acta Neuropathol Commun. 2022;10(1):165. doi: 10.1186/s40478-022-01469-7.