Experimental Models Of Metabolic Syndrome In Male Wistar Rats Tropical Journal of Natural Product Research
Main Article Content
Abstract
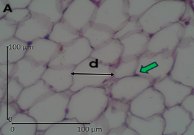
Metabolic syndrome’s prevalence ranges from 20-25% of the adult population. It is reported to elevate the risk of cardiovascular diseases, stroke, and several cancers. Establishing an animal model of metabolic syndrome is crucial to evaluating treatment modalities. This research aimed to compare various methods of inducing metabolic syndrome. A study with pre and post-only with a control group design, combined with post-test only with a control group was conducted on 20 male Wistar rats. At the baseline, anthropometric and biochemical parameters were evaluated. Animals were then randomly allocated into four comparable groups, group I (control); group II(dexamethasone), group III: fructose and dexamethasone combination; and hight-fat-diet combined with fructose drinking water (group IV). Dexamethasone was given at 1 mg/kg/day intraperitoneally, fructose was provided ad libitum as 20% fructose drinking water (FDW), while the high-fat diet were given as egg yolk and repeatedly heated vegetable oil (1:1). All treatments were given for 10 days. After interventions, all parameters were re-evaluated and histologic analyses were performed. Group II and III developed systolic hypertension, and elevated glucose and cholesterol levels, but no changes in adipocyte diameter and obesity index. A high-fat diet combined with 20% FDW groups showed weight gain, elevated diastolic blood pressure and glucose levels, and also slight lipohypertrophy. We concluded that treatment with dexamethasone and fructose-dexamethasone combination mimicked the metabolic parameters but not the obesity traits. The high-fat-fructose group was shown to induce lipohypertrophy but not lipohyperplasia.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
1. Dobrowolski P, Prejbisz A, Kurlowicz A, Baska A, Burcahrdt P, Chlebus K, Dzida G, Jankowski P. Jaroszewicz J, Jaworski P, Kaminski K, Kaplon-Cieslicka A, Klocek M, Kukla M, Mamcarz A, Mastalerz-Migas A, Narkiewics K, Ostrowska L, Sliz D, Tarnowski W, Wolf J, Wylezol M, Zdrojewski T, Banach M, Januszewicz A, Bogdanski P. Metabolic Syndrome-A New Definition and Management Guidelines. Arch Med Sci. 2022;18(5):1133–1156. DOI: 10.5114/aoms/152921.
2. Fahed G, Aoun L, Zerdan MB, Allam S, Zerdan MB, Bouferraa Y, Assi HI. Metabolic Syndrome: Updates on Pathophysiology and Management in 2021. Int J Mol Sci. 2022; 23, 786:1-38. https://doi.org/10.3390/ijms23020786
3. Saklayen MG. The Global Epidemic of the Metabolic Syndrome. Curr Hypertens Rep. 2018;20(12):1–8. https://doi.org/10.1007/s11906-018-0812-z
4. Ranasinghe P, Mathangasinghe Y, Jayawardena R, Hills AP, Misra A. Prevalence and Trends of Metabolic Syndrome Among Adults in The Asia-pacific Region: A Systematic Review. BMC Public Health. 2017; 21;17(101):1-9. DOI 10.1186/s12889-017-4041-1
5. Herningtyas EH, Ng TS. Prevalence and Distribution of Metabolic Syndrome and Its Components Among Provinces and Ethnic Groups in Indonesia. BMC Public Health. 2019;19(377):1–12. https://doi.org/10.1186/s12889-019-6711-7
6. Li W, Qiu X, Ma H, Geng Q. Incidence and Long-Term Specific Mortality Trends of Metabolic Syndrome in the United States. Front Endocrinol (Lausanne). 2023;13:1029736. https://doi.org/10.3389/fendo.2022.1029736
7. Yang C, Jia X, Wang Y, Fan J, Zhao C, Yang Y, Shi X. Trends and Influence Factors in The Prevalence, Intervention, and Control of Metabolic Syndrome among US Adults, 1999–2018. BMC Geriatr. 2022;22(1):979. https://doi.org/10.1186/s12877-022-03672-6
8. Neill SO, Driscoll LO. Metabolic syndrome: A Closer Look at The Growing Epidemic and Its Associated Pathologies. Obesity Reviews. 2015;16:1–12. DOI: 10.1111/obr.12229
9. Machado-Fragua MD, Fayosse A, Yerramalla MS, van Sloten TT, Tabak AG, Kivimaki M, Sabia S, Singh-Manoux A. Association of Metabolic Syndrome With Incident Dementia: Role of Number and Age at Measurement of Components in a 28-Year Follow-up of the Whitehall II Cohort Study. Diabetes Care. 2022 ;45(9):2127–2135. https://doi.org/10.2337/dc22-0206
10. Dobrowolski P, Prejbisz A, Kurylowicz A, Baska A, Burchardt P, Chlebus K Dzida G, Jankowski P. Jaroszewicz J, Jaworski P, Kaminski K, Kaplon-Cieslicka A, Klocek M, Kukla M, Mamcarz A, Mastalerz-Migas A, Narkiewics K, Ostrowska L, Sliz1 D, Tarnowski W, Wolf J, Wylezol M, Zdrojewski T, Banach M, Januszewicz A, Bogdanski P. Metabolic Syndrome: A New Definition and Management Guidelines. Arch Med Sci. 2022;18(5):1133–1156. DOI: https//doi.org/10.5114/aoms/152921
11. Uzunlulu M, Telci O, Aytekin C. Association Between Metabolic Syndrome and Cancer. Ann Nutr Metab. 2016;(68):173–179. DOI: 10.1159/000443743
12. Ashique S, Upadhyay A, Kumar N, Chauhan S, Mishra N. Metabolic Syndromes Responsible for Cervical Cancer and Advancement of Nanocarriers for Efficient Targeted Drug Delivery-A review. Adv Cancer Biol- Met. 2022; 100041. https://doi.org/10.1016/j.adcanc.2022.100041
13. Paley CA, Johnson MI. Abdominal Obesity And Metabolic Syndrome: Exercise as Medicine ? BMC Sports Sci Med Rehabil. 2018;10(7):1–8. https://doi.org/10.1186/s13102-018-0097-1
14. Zhou X, Han D, Xu R, Li S, Wu H, Qu C, Wang F, Wang X, Zhao Y. A Model of Metabolic Syndrome and Related Diseases with Intestinal Endotoxemia in Rats Fed a High Fat and High Sucrose Diet. PLoS One. 2014;9(12):e115148:1–22. https://doi.org/10.1371/journal.pone.0115148
15. Wong SK, Chin KY, Suhaimi FH, Fairus A, Ima-Nirwana S. Animal Models of Metabolic Syndrome: A Review. Nutr Metab (Lond). 2016;13:65:1–12. DOI: 10.1186/s12986-016-0123-9.
16. Gunawan S, Aulia A, Soetikno V. Development of Rat Metabolic Syndrome Models: A Review. Vet World. 2021;14(7): 1774–1783. DOI: 10.14202/vetworld.2021.1774-1783
17. Mamikutty N, Thent ZC, Sapri SR, Sahruddin NN, Mohd Yusof MR, Suhaimi HF. The Establishment of Metabolic Syndrome Model by Induction of Fructose Drinking Water in Male Wistar Rats. Biomed Res Int. 2014;263897:1-8. http://dx.doi.org/10.1155/2014/263897
18. Moreno-Fernández S, Garcés-Rimón M, Vera G, Astier J, Landrier JF, Miguel M. High Fat/High Glucose Diet Induces Metabolic Syndrome in An Experimental Rat Model. Nutrients. 2018;14;10(10):1502-1517. DOI: 10.3390/nu10101502.
19. Askar M, Ibrahim I, Mahmoud M. Dexamethasone-Induced Metabolic Syndrome: Re-Evaluation of An Underestimated Experimental Model. Bull Pharm Sci. 2022;45(2):989-1004. Available from: 10.21608/bfsa.2022.271784
20. Arifin WN, Zahiruddin WM. Sample Size Calculation in Animal Studies Using Resource Equation Approach. Malays J Med Sci. 2017;24(5):101–105. DOI: 10.21315/mjms2017.24.5.11.
21. Kumar SR, Ramli ESM, Nasir NAA, Ismail NM, Fahami NAM. Methanolic Extract of Piper Sarmentosum Attenuates Obesity and Hyperlipidemia in Fructose-Induced Metabolic Syndrome Rats. Molecules. 2021;26(13). DOI: 10.3390/molecules26133985
22. Mamikutty N, Thent ZC, Suhaimi FH. Fructose-Drinking Water Induced Nonalcoholic Fatty Liver Disease and Ultrastructural Alteration of Hepatocyte Mitochondria in Male Wistar Rat. Biomed Res Int. 2015;2015:895961. DOI: 10.1155/2015/895961.
23.Luong Q, Huang J, Lee KY. Deciphering White Adipose Tissue Heterogeneity. Biology (Basel). 2019;8(2):1-14. DOI: 10.3390/biology8020023
24. Arnoldussen IAC, Zerbi V, Wiesmann M, Noordman RHJ, Bolijn S, Mutsaers MPC, Dederen PJWC, Kleemann R, Kooistra T, van Tol EAF, Gross G, Schoemaker MH, Heerschap A, Wielinga PY , Kiliaan AJ. Early Intake of Long-Chain Polyunsaturated Fatty Acids Preserves Brain Structure and Function in Diet-Induced Obesity. J Nut Biochem. 2016;30:177–188. DOI: 10.1016/j.jnutbio.2015.12.011.
25. Oche J, Olorundare O, Afolabi S, Ologe M, Njan A, Akanbi O. Comparative Therapeutic Effect of Single/Combined Administration of Saxagliptin, Metformin and Intranasal Insulin on Dexamethasone Induced Insulin Resistance in Wistar Rat Model. Niger J Physiol Sci. 2023;38(1):37–46. DOI: 10.54548/njps.v38i1.7.
26. Koorneef LL, van der Meulen M, Kooijman S, Sánchez-López E, Scheerstra JF, Voorhoeve MC, Ramesh ANN, Rensen PCN, Giera M, Kroon J, Meijer OC. Dexamethasone-Associated Metabolic Effects in Male Mice are Partially Caused by Depletion of Endogenous Corticosterone. Front Endocrinol (Lausanne). 2022 ;13: 960279. DOI: 10.3389/fendo.2022.960279
27. Shittu STT, Ogundele OJ, Shittu SA, Isehunwa GO, Afolabi AO, Lasisi TJ. Dexamethasone Induction of Metabolic Syndrome and Remediation By Medicinal Plants: A Systematic Review. Trop J Nat Prod Res. 2024. 8(8): 7930–7940. https://doi.org/10.26538/tjnpr/v8i8.1.
28. Pereira GA, Sodré FS, Murata GM, Amaral AG, Payolla TB, Campos CV, Sato FT, Anhe GF, Bordin S. Fructose Consumption by Adult Rats Exposed to Dexamethasone in Utero Changes The Phenotype of Intestinal Epithelial Cells and Exacerbates Intestinal Gluconeogenesis. Nutrients. 2020;1;12(10):1–17. DOI:10.3390/nu12103062
29. Shalam M, Harish M, Farhana S. Prevention of Dexamethasone-and Fructose-Induced Insulin Resistance in Rats by SH-01D, a Herbal preparation. Indian J Pharmacol. 2006;38(6):419–422. DOI: 10.4103/0253-7613.28209
30. Ferreira SRD, Pessoa RF, Figueiredo IAD, Lima JPM, de Moura TMCF, Bezerra CO, de Oliviera Martins AM, de Carvalho LM, Madruga MS, Cavalcante HC, de Souza Aquino J, de Brito Alves JL, Alves AF, Vasconcelos LHC, de Andrade Cavalcante F. Functional and Morphologic Dysfunctions in The Airways of Rats Submitted to An Experimental Model of Obesity-Exacerbated Asthma. Sci Rep. 2022;12(1): 9540. DOI: 10.1038/s41598-022-13551-0
31. Malkawi AK, Alzoubi KH, Jacob M, Matic G, Ali A, Al Faraj A Almuhana F, Dasouki M, Rahman AMA. Metabolomics Based Profiling of Dexamethasone Side Effects in Rats. Front Pharmacol. 2018;16;9:46. DOI: 10.3389/fphar.2018.00046.
32. Wang L, Wang H, Zhang B, Popkin BM, Du S. Elevated Fat Intake Increases Body Weight and The Risk of Overweight and Obesity Among Chinese Adults: 1991–2015 trends. Nutrients. 2020;12(11):3272-3285. DOI: 10.3390/nu12113272.
33. Azevedo-Martins AK, Santos MP, Abayomi J, Ferreira NJR, Evangelista FS. The Impact of Excessive Fructose Intake on Adipose Tissue and the Development of Childhood Obesity. Nutrients. 2024;16(7):939-956. https://doi.org/10.3390/nu16070939
34. Herrera NA, Duchatsch F, Kahlke A, Amaral SL, Vasquez-Vivar J. In Vivo Vascular Rarefaction And Hypertension Induced by Dexamethasone are Related to Phosphatase PTP1B Activation Not Endothelial Metabolic Changes. Free Radic Biol Med. 2020.152:689–696. DOI: 10.1016/j.freeradbiomed.2020.01.012
35. Janssen LEF, Simons N, Simons PIHG, Schaper NC, Feskens EJM, van der Ploeg LMC, van der Eynde M, Schalkwijk CG, Houben AJHM, Stehouwer CDA, Brouwers MCGJ. Effects of Fructose Restriction on Blood Pressure: Secondary Analysis of A Double-Blind Randomized Controlled Trial. Clin Nutr ESPEN. 2022;51:97–103. DOI: 10.1016/j.clnesp.2022.07.009
36. Logvinov S, Naryzhana VN, Kurbatov B, Gorbunov A, Birulina Y, Maslov L, Oeltgen PR. High Carbohydrate High Fat Diet Causes Arterial Hypertension and Histological Changes in The Aortic Wall. Exp Gerontol. 2021;154: 111543, 1–12. DOI: 10.1016/j.exger.2021.111543
37. Martínez BB, Pereira ACC, Muzetti JH, de Paiva Telles F, Mundim FGL, Teixeira MA. Experimental Model of Glucocorticoid-Induced Insulin Resistance. Acta Cir Bras. 2016;31(10):645–649. DOI: 10.1590/S0102-865020160100000001
38. Purushothaman AM, Pujari VS, Kadirehally NB, Bevinaguddaiah Y, Reddy PR. A Prospective Randomized Study on The Impact Of Low-Dose Dexamethasone on Perioperative Blood Glucose Concentrations in Diabetics and Nondiabetics. Saudi J Anaesth. 2018;12(2):198–203. DOI: 10.4103/sja.SJA_409_17.
39. Jalilvand A, Behrouz V, Nikpayam O, Sohrab G, Hekmatdoost A. Effects of Low Fructose Diet on Glycemic Control, Lipid Profile and Systemic Inflammation in Patients With Type 2 Diabetes: A Single-Blind Randomized Controlled Trial. Diabetes Metab Syndr:Clinical review. 2020;14:849–855. DOI: 10.1016/j.dsx.2020.04.003
40. Giussani M, Lieti G, Orlando A, Parati G, Genovesi S. Fructose Intake, Hypertension and Cardiometabolic Risk Factors in Children and Adolescents: From Pathophysiology to Clinical Aspects. A Narrative Review. Front Med (Lausanne).2022:9:792949. DOI: 10.3389/fmed.2022.792949.
41. Abdou M, Hafez M, Anwar G, Fahmy W, Abd AlFattah N, Salem R, Arafa N. Effect of High Protein And Fat Diet on Postprandial Blood Glucose Levels. Diabetes Metab Syndr. 2021;15 (1):7–12. DOI: 10.1016/j.dsx.2020.11.020
42. Strober JW, Fernandez S, Ye H, Brady MJ. Differential Effects of Acute Versus Chronic Dietary Fructose Consumption on Metabolic Responses in FVB/N Mice. Am J Physiol Regul Integr Comp Physiol. 2022 1;323(2):R255–R266. DOI: 10.1152/ajpregu.00174.2021.
43. Maharjan BR, McLennan S V, Yee C, Twigg SM, Williams PF. The Effect of A Sustained High-Fat Diet on The Metabolism of White and Brown Adipose Tissue and Its Impact on Insulin Resistance: A Selected Time Point Cross-Sectional Study. Int J Mol Sci. 2021;22(24). 13639. DOI: 10.3390/ijms222413639.
44. Barclay JL, Agada H, Jang C, Ward M, Wetzig N, Ho KKY. Effects of Glucocorticoids on Human Brown Adipocytes. J Endocrinol. 2015;224(2):139–147. DOI: 10.1530/JOE-14-0538
45. Zhang H, Ke W, Chen X, Han Y, Xiong Y, Zhu F, Xiang Y, Yang R, Cai H, Huang S, Ke X. High-Fat Diet Promotes Adipogenesis in Offspring Female Rats Induced by Perinatal Exposure to 4-Nonylphenol. Biomed Res Int. 2023; 2023:6540585. DOI: 10.1155/2023/6540585
46. Crescenzo R, Bianco F, Coppola P, Mazzoli A, Valiante S, Liverini G, Iossa S. Adipose Tissue Remodeling in Rats Exhibiting Fructose-Induced Obesity. Eur J Nutr. 2014;53(2):413–419. DOI: 10.1007/s00394-013-0538-2.