Renal Function Indices of Ulcerated Rats Pre-Treated with Binary Combinations of Persea americana Seed and Bryophyllum pinnatum Leaf Ethyl Acetate Fraction
Main Article Content
Abstract
The use of certain medications and herbal remedies poses a significant risk to renal function. The study aimed to investigate the effect of binary combinations of Persea americana seed (PAEF) and Bryophyllum pinnatum leaf (BPEF) ethyl acetate fractions on renal function indices of ulcerated rats. Wistar rats were divided into ten groups of five rats each. The groups were designated: normal control (NC) (Group 1), ulcer control (UC) (Group 2), Omeprazole (OMEP) (Group 3), PAEF (Group 4), BPEF (Group 5), PAEF + BPEF (1:1) (Group 6), PAEF + BPEF (1:2) (Group 7), PAEF + BPEF (1:3) (Group 8), PAEF + BPEF (2:1) (Group 9), and PAEF + BPEF (3:1) (Group 10). Groups 4-10 were pre-treated with 400 mgkg-1 body weight/day of ethyl acetate fractions of the plants, and their binary combinations orally for 21 days. On the 22nd day, after 12 h fasting, gastric ulcer was induced in the rats in groups 2-10 by a single oral dose of indomethacin (30 mg/kg body weight). Results showed that the administration of PAEF + BPEF (1:2), PAEF + BPEF (1:3), PAEF + BPEF (2:1), PAEF + BPEF (3:1), and omeprazole caused significant (p<0.05) elevation of serum urea when compared to NC and UC. The binary combinations PAEF + BPEF (1:1), PAEF + BPEF (1:3), PAEF + BPEF (2:1), PAEF + BPEF (3:1) caused normalization of serum calcium, magnesium, and zinc concentrations comparable to normal control. Therefore, the binary combinations of PAEF and BPEF may distort kidney function and electrolyte balance.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
How to Cite
References
1. Xie X, Ren K, Zhou Z, Dang C, Zhang H. The global, regional and national burden of peptic ulcer disease from 1990 to 2019: a population-based study. BMC Gastroenterol 2022; 22:58.
2. Salari N, Darvishi N, Shohaimi S, Bartina Y, Ahmadipanah M, Salari HR, Mohammadi M. The Global Prevalence of
Peptic Ulcer in the World: a Systematic Review and Meta-analysis. Indian J Surg. 2022; 84:913–921.
3. Cai S, Garcia-Rodriguez LA, Masso-Gonzalez EL, Hernandez-Diaz S. Uncomplicated peptic ulcer in the UK: trends from 1997 to 2005. Alimen Pharmacol Ther. 2009; 30: 1039–1048.
4. Xing-Zi L, Yue-Miao Z, Ni-Ya J, Hong Z. Helicobacter pylori infection is associated with elevated galactose-deficient IgA1 in IgA nephropathy. Ren Fail. 2020; 42(1):539-546.
5. Wei Pan, H, Li W, Tingting Z, Bo C, Junming F. Association between Helicobacter pylori infection and kidney damage in patients with peptic ulcer. Ren Fail. 2019; 41(1):1028-1034.
6. Sari TA, Nadir AI, Areej AA, Hatim MM, Hamza MA, Hassan AH, Yahya AA, Waleed HM, Khalid OA. Acute Helicobacter pylori infection prevalence among renal failure Pptients and its potential roles with other chronic diseases: A retrospective cohort study. Infect Drug Resis. 2022; 15:6589-6599.
7. Lucas GNC, Leitão ACC, Alencar RL, Xavier RMF, Daher EF, Silva Junior GBD. Pathophysiological aspects of nephropathy caused by non-steroidal anti-inflammatory drugs. J Brasil Nefro. 2019; 41(1):124–130.
8. Kim S, Joo KW. Electrolyte and Acid-base disturbances associated with non-steroidal anti-inflammatory drugs. Electro. Blood Press. 2007; 5:116–125.
9. Harirforoosh S, Asghar W, Jamali F. Adverse effects of nonsteroidal anti-inflammatory drugs: an update of gastrointestinal, cardiovascular and renal complications. J Pharm Pharm Sci. 2013; 16:821–847.
10. Asiwe ES, Igwe CU, Iheanacho KM, Onyeocha IO, Onwuliri VA. Bioactive composition and acute oral toxicity studies on
Persea americana seed ethyl acetate fraction. Asian J Res Biochem. 2021a; 8(4):10-17.
11. Sokpe A, Mensah MLK, Koffuor GA, Thomford KP, Arthur R, Jibira Y, Baah MK, Adedi B, Agbemenyah HY. Hypotensive and antihypertensive properties and safety for use of Annona muricata and Persea americana and their combination products. Evid-Based Compliment Altern Med. 2020; 2020(6):1-13.
12. Makelele F, Mukweke N, Hamuli M, Kadima J, Bwironde F, Chasinge T, Murhula H. Antiulcer effect of Persea americana seed against alcohol-induced peptic ulcer in guinea pig. J Pharm Phytochem. 2020; 9(4):1244-1249.
13. Alkhalaf MI, Alansari WS, Ibrahim EA, ELhalwagy MEA. Anti-oxidant, anti-inflammatory, and anti-cancer activities of avocado (Persea americana) fruit and seed extract. J King Saud Univ. 2019; 31(4):1358-1362.
14. Fernandes JM, Cunha LM, Azevedo EP, Lourenço EMG, Fernandes-Pedrosa MF, Zucolotto SM. Kalanchoe laciniata and Bryophyllum pinnatum: an updated review about ethnopharmacology, phytochemistry, pharmacology and toxicology. Rev Brasil Farmacog. 2019; 29 (4):529-558.
15. Andrade AWL, Guerra GCB, de Souza-Araújo DF, de Araújo-Júnior RF, de Araújo AA, de Carvalho TG, Fernandes JM, Diez-Echave P, Hidalgo-García L, Rodriguez-Cabezas ME, Gálvez J, Zucolotto SM. Anti-inflammatory and chemopreventive effects of Bryophyllum pinnatum (Lamarck) leaf extract in experimental colitis models in rodents. Front Pharmacol. 2020; 11(7):1-18.
16. Emenike BA, Emmanuel CO, Obiora CU, Valentine ON, Chioma AA, Petra ON, Okwesili FCN. Ulcer-protective property of Bryophyllum pinnatum leaf extract and their phytosomal formulations. Trop J Nat Prod Res. 2020; 4(12):1201-1207.
17. Asiwe ES, Igwe CU, Onwuliri VA, Iheanacho KME, Iheanacho JN. Characterization of Chemical Composition of Bryophyllum pinnatum leaf ethyl acetate fraction. Asian J Adv Res Rep. 2021b; 15(4):15-24.
18. Asiwe ES, Igwe CU, Iheanacho KME, Onyeocha IO, Onwuliri VA. Antioxidative and Free radical scavenging properties of ethyl acetate fractions of Persea americana seed and Bryophyllum pinnatum leaf. Trop J Nat Prod Res. 2021c; 5(8):1486-1492.
19. Asiwe ES, Igwe CU, Iheanacho KME, Onwuliri VA, Alisi CS, Ezeji-Chigbu NG, Ujowundu CO. Ulcero-protective potential of ethyl acetate fractions of Persea americana seed and Bryophyllum pinnatum leaf binary combinations in indomethacin induced gastric ulcer. Asian J Biochem Gen Mol Biol. 2022; 12(4):139-153.
20. Hsieh C, Huang S, Chen CL, Chen W, Chang HC, Wu ML, Yang CC. Increased risk of chronic kidney disease among users of non-prescribed Chinese herbal medicine in Taiwan. Prev Med. 2012; 55: 155-159.
21. Asiwe ES, Ugenyi AU, Enenebeaku UE, Opara PO, Alisi CS, Ekezie J. (2023). Changes in hepatic function indices in ulcerated rats treated with persea americana seed and Bryophyllum pinnatum leaf ethyl acetate fraction. Trop J Nat Prod Res. 2023; 7(9):4084-4091.
22. Searcy RL, Reardon JE, Foreman JA. A new photometric method for serum urea nitrogen determination. Am J Med Technol. 1967; 33(1):15–20.
23. Bartels H, Boehmer M. Micro-determination of creatinine. Clin Chem Acta. 1971; 32:81-85.
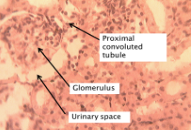
24. Fabiny DL, Ertingshausen G. Automated reaction-rate method for determination of serum creatinine with the CentrifiChem. Clin Chem. 1971; 17(8):696–700.
25. Terri AE, Sesin PG. Determination of serum potassium by using sodium tetraphenylboro method. Am J Clin Pathol. 1958; 29(1):86-90.
26. Skeggs LT, Hochstrasser H. Multiple Automatic Sequential
Analysis. Clin Chem. 1964; 10:918–936.
27. Maruna RF. Serum sodium determination; critical study on colorimetric determination and method. Inter. J Clin Chem. 1957; 2(6):581–585.
28. Trinder P. A rapid method for the determination of sodium in serum. Analyst. 1951; 76:596-599.
29. Kaplan LA, Glucose KA. Clinical Chemistry. The C. V. Mosby Co. St Louis. Toronto. Princeton. 1974; 1032-1036 .
30. Gindler EM, King JD. Rapid colorimetric determination of calcium in biologic fluids with methylthymol blue. Am J Clin Pathol. 1972; 58(4):376–382.
31. Chauman UPS, Ray SBC. Use of Calmagite for the determination of traces of magnesium in biological materials. Anal Biochem. 1969; 13(1):70-80.
32. Abe A, Yiamashita S, Noma A. Sensitive, direct colourimetric method for copper in serum. Clin Chem. 1989; 35(4):552-554.
33. Makino T. A sensitive, direct colorimetric assay of serum zinc using nitro-PAPS and microwell plates. Clin Chim Acta. 1991; 197(3):209-220.
34. Abebe MS, Gebru G. Toxic effect of Vernonia amygdalina Delile on blood parameters and histopathology of liver and kidney in rats. Global J Med Plants Res. 2015; 1(1):001-008.
35. Mehmood HR, Khan Z, Jahangir HMS, Hussain A, Elahi A, Askari SMH. Assessment of serum biochemical derangements and associated risk factors of chronic kidney disease. J Taibah Univ Med Sci. 2021; 17(3):376-383.
36. Mercado MG, Smith DK, Guard EL. Acute Kidney Injury: Diagnosis and Management. Am Fam Phy. 2019; 100(11):687–694.
37. Carvalho MHC, Nigro D, Lemos VS, Tostes RCA, Fortes ZB. Arterial hypertension: the endothelium and its multiple functions/Arterial hypertension: endothelium and multiple functions. Rev. Brasil. Med. 2001; 8(1):76–88.
38. AlShanableh Z, Ray EC. Magnesium in hypertension: mechanisms and clinical implications. Front Physiol. 2024; 15:1363975.
39. Saini HK, Tripathi ON, Zhang S, Elimban V, Dhalla NS. Involvement of Na+/Ca2+ exchanger in catecholamine-induced increase in intracellular calcium in cardiomyocytes. Am J Physiol Circul Physiol. 2006; 290:373–380.
40. Kamal F, Khan MA, Molnar MZ, Howden CW. The Association Between Proton Pump Inhibitor Use with Acute Kidney Injury and Chronic Kidney Disease. J Clin Gastroenterol. 2018; 52:468–476.
41. Gommers LMM, Hoenderop JGJ, de Baaij JHF. Mechanisms of proton pump inhibitor-induced hypomagnesemia. Acta Physiol. 2022; 235(4):e13846.
42. Cheungpasitporn W, Thongprayoon C, Kittanamongkolchai W, Srivali N, Edmonds PJ, Ungprasert P, O'Corragain OA, Korpaisarn S, Erickson SB. Proton pump inhibitors linked to hypomagnesemia: a systematic review and meta-analysis of observational studies. Ren Fail. 2015; 37(7):1237–1241.
43. Qiu T, Zhou J, Zhang C. Acid-suppressive drugs and risk of kidney disease: A systematic review and meta-analysis. J Gastroenterol Hepatol. 2018; 10.1111/jgh.14157.
44. Nabavi-Rad A, Azizi M, Jamshidizadeh S, Sadeghi A, Aghdaei HA, Yadegar A, Zali MR. The Effects of Vitamins and Micronutrients on Helicobacter pylori Pathogenicity, Survival, and Eradication: A Crosstalk between Micronutrients and Immune System. J Immunol Res. 2022; 2022:4713684.
45. Namikawa T, Utsunomiya M, Yokota K, Munekage M, Uemura S, Maeda H, Kitagawa H, Kobayashi M, Hanazaki K. Association between Serum Zinc Levels and Clinicopathological Characteristics in Patients with Gastric Cancer. Gastrointest Tumors. 2023;10(1):6-13.
46. Meng-Chieh W, Chun-Yi H, Fu-Chen K, Wen-Hung H, Sophie SW, Hsiang-Yao S, Chung L. Chien-Yu L. The
Effect of Helicobacter pylori eradication on the levels of essential trace elements. Biomed Res Int. 2014; 2014:5-15.
47. Wessels I, Rolles B, Rink L. The potential impact of zinc supplementation on COVID-19 pathogenesis. Front Immunol. 2020; 11:1712.
48. Dovhanj J, Kljaic K, Dodig-Curkovic, K, Curkovic M, Volarevic M, dMarjanovic K. Helicobacter Pylori, Zinc and Iron in Oxidative Stress-Induced Injury of Gastric Mucosa”, Mini-Rev Med Chem. 2009; 9(1):26-30.
49. Christudoss P, Fleming J. Mathew G. Zinc levels in paired normal and malignant human stomach and colon tissue. Biomed Res. 2010; 21(4):445-450.
50. Pacifici GM. Differential renal adverse effects of ibuprofen and indomethacin in preterm infants: a review. Clin Pharmacol: Adv Appl. 2014; 6:111–116.
51. Lee CH, Chen HN, Tsao LY, Hsiao CC, Lee ML. Oral ibuprofen versus intravenous indomethacin for closure of patent ductus arteriosus in very low birth weight infants. Ped Neonat. 2012; 53:346–353.
52. Wongrakpanich S, Wongrakpanich A, Melhado K, Rangaswami J. A Comprehensive Review of Non-Steroidal Anti-Inflammatory Drug Use in the Elderly. Aging Dis. 2018; 9(1):143–150.
53. Lazarus B, Chen Y, Wilson FP, Sang Y, Chang AR, Coresh J, Grams ME. Proton Pump Inhibitor Use and the Risk of
Chronic Kidney Disease. JAMA Int Med. 2016; 176(2):238–246.
54. Xie Y, Bowe B, Li T, Xian H, Balasubramanian S, Al-Aly, Z. Proton Pump Inhibitors and Risk of Incident CKD and Progression to ESRD. J Am Soc Nephrol. 2016; 27:3153-3163.
55. Morschel CF, Mafra D, Eduardo J. The relationship between proton pump inhibitors and renal disease. J Brasil Nefrol. 2018; 40(3):301–306.
56. Guedes JV, Aquino JA, Castro TL, Augusto de Morais F, Baldoni AO, Belo VS, Otoni A. Omeprazole use and risk of chronic kidney disease evolution. PloS One. 2020; 15(3):e0229344.
57. Zheltova AA, Kharitonova MV, Iezhitsa IN, Spasov AA. Magnesium deficiency and oxidative stress: an update. Biomed (Taipei). 2016; 6(4):20.