Differentially Expressed Genes (DEGs) Analysis and <I>In Silico</I> Studies Identify Tumor Necrosis Factor (TNF) Inhibition and Peroxisome Proliferator-Activated Receptor Alpha (PPARA) Activation as Targets for Gallic Acid Derivatives in Insulin Resistance
Main Article Content
Abstract
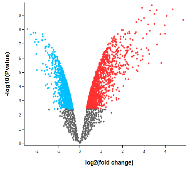
Insulin resistance is a critical factor in developing metabolic disorders like type 2 diabetes, posing challenges for effective treatment. Identifying molecular targets to reverse or mitigate insulin resistance is a key focus in therapeutic research. Advances in genomics and bioinformatics have enabled researchers to explore differentially expressed genes (DEGs) as potential biomarkers and therapeutic targets. This study aims to identify potential therapeutic targets for overcoming insulin resistance based on the analysis of (DEGs). Gallic acid (GA) and its derivatives were then tested against these identified targets using in silico methods. DEGs were analyzed from two Gene Expression Omnibus (GEO) datasets: GSE13070 (human adipose tissue with insulin resistance and insulin sensitivity) and GSE24422 (TNF-induced and non-induced adipocyte cell culture). The identified DEGs were then compared to find common DEGs, which were subsequently analyzed to identify hub-genes. Cross-validation using neural network and principal component analysis (PCA) on gene expression values revealed that the identified hub-genes, including IRS1, PCK1, GYS1, PTRPF, ACACB, and PIK3R2, can serve as biomarkers for insulin resistance (area under the curve, AUC 0.956 and sensitivity 1.00). The search for upstream regulatory proteins (URPs) of the hub-genes in the Comparative Toxicogenomics Database indicated that the activities of TNF, PPARA, and AHR could influence the expression of several hub-genes, namely IRS1, PCK1, and ACACB. The activity prediction analysis, which was based on SkelSpheres molecular descriptors and confirmed by molecular docking, suggests that caffeoyl gallic acid may be a candidate compound for overcoming insulin resistance by inhibiting TNFA and activating PPARA.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
Szablewski L. Changes in Cells Associated with Insulin Resistance. Int J Mol Sci. 2024; 25:2397-2424. https://doi.org/10.3390/ijms25042397.
Chaoji SA. Insulin Resistance. Vidarbha J Intern Med. 2023; 33:27-31. https://doi.org/10.25259/VJIM_41_2022.
Singh A, Ghai N, Mohinder Singh Bedi P. Molecular Mechanisms Involved in Insulin Resistance: Recent Updates and Future Challenges. Evolving Concepts in Insulin Resistance, IntechOpen; 2022. https://doi.org/10.5772/intechopen.104806.
Calcaterra V, Zuccotti G, Mari A, Iafusco F, Maione G, Iafusco D, Tinto N. Can obesity exacerbate hyperinsulinaemia in the presence of the mutation of an insulin receptor gene? Clin Obes. 2023; 13:e12619-e12627. https://doi.org/10.1111/cob.12619.
Bhattacharjee A, Pranto SMAM, Ahammad I, Chowdhury ZM, Juliana FM, Das KC, Keya CA, Salimullah M. High risk genetic variants of human insulin receptor substrate 1(IRS1) infer structural instability and functional interference. J Biomol Struct Dyn. 2023; 41:15150–64. https://doi.org/10.1080/07391102.2023.2187232.
Song Y, Li S, He C. PPARγ Gene Polymorphisms, Metabolic Disorders, and Coronary Artery Disease. Front Cardiovasc Med. 2022; 9:808929-808941. https://doi.org/10.3389/fcvm.2022.808929.
Elangeeb ME, Elfaki I, Elkhalifa MA, Adam KM, Alameen AO, Elfadl AK, Albalawi IA, Almasoudi KS, Almotairi R, Alsaedi BSO, Alhelali MH, Mir MM, Amle D, Mir R. In Silico Investigation of AKT2 Gene and Protein Abnormalities Reveals Potential Association with Insulin Resistance and Type 2 Diabetes. Curr Issues Mol Biol. 2023; 45:7449–7475. https://doi.org/10.3390/cimb45090471.
van Gerwen J, Shun-Shion AS, Fazakerley DJ. Insulin signalling and GLUT4 trafficking in insulin resistance. Biochem Soc Trans. 2023; 51:1057–1069. https://doi.org/10.1042/BST20221066.
Baheej MAA, Haniffa HM, Siddiqui H, Jabeen A. Synthesis and biological evaluation of gallic acid esters as phagocyte oxidative burst inhibitors. J Natl Sci Found. 2023; 51:415–421. https://doi.org/10.4038/jnsfsr.v51i3.11199.
Saini A, Saini VD, Saharan R, Kumar S. Gallic Acid: A Wonderful Remedy in Medicinal Field. Curr Tradit Med. 2023; 10:1-17 https://doi.org/10.2174/0122150838266828231005055236.
Errabiti B, El Aabedy A, Er-Rahmani S, El Abed S, Koraichi SI. Antimicrobial Effects of Tannic and Gallic Acids: A Study on 3D-Printed Polylactic Acid Surfaces Against P. aeruginosa and S. aureus. Trop J Nat Prod Res. 2024; 8(10):8753 -8763. https://doi.org/10.26538/tjnpr/v8i10.18.
Vu D. Assessing the Differences in Phenolics, Antioxidant and Anti-Tyrosinase Activities of Spent Coffee Ground Fractions . Trop J Nat Prod Res. 2022; 6(4):558-562
Doan KV, Ko CM, Kinyua AW, Yang DJ, Choi YH, Oh IY, Nguyen NM, Ko A, Choi JW, Jeong Y, Jung MH, Cho WG, Xu S, Park KS, Park WJ, Choi SY, Kim HS, Moh SH, Kim KW. Gallic acid regulates body weight and glucose homeostasis through AMPK activation. Endocrinology. 2015; 156:157–168. https://doi.org/10.1210/en.2014-1354.
Makihara H, Koike Y, Ohta M, Horiguchi-Babamoto E, Tsubata M, Kinoshita K, Akase T, Goshima Y, Aburada M, Shimada T. Gallic Acid, the Active Ingredient of Terminalia bellirica, Enhances Adipocyte Differentiation and Adiponectin Secretion. Biol Pharm Bull. 2016; 39:1137–1143. https://doi.org/10.1248/bpb.b16-00064.
Shakoor H, Hussein H, Al-Hassan N, Alketbi M, Kizhakkayil J, Platat C. The Muscle-Conditioned Medium Containing Protocatechuic Acid Improves Insulin Resistance by Modulating Muscle Communication with Liver and Adipose Tissue. Int J Mol Sci. 2023; 24:9490-9511. https://doi.org/10.3390/ijms24119490.
Ul Haq Shah MZ, Soni M, Shrivastava VK, Mir MA, Muzamil S. Gallic acid reverses ovarian disturbances in mice with letrozole-induced PCOS via modulating Adipo R1 expression. Toxicol Rep. 2022; 9:1938–1949. https://doi.org/10.1016/j.toxrep.2022.10.009.
Barrett T, Wilhite SE, Ledoux P, Evangelista C, Kim IF, Tomashevsky M, Marshall KA, Phillippy KH, Sherman PM, Holko M, Yefanov A, Lee H, Zhang N, Robertson CL, Serova N, Davis S, Soboleva A. NCBI GEO: archive for functional genomics data sets--update. Nucleic Acids Res. 2013; 41:D991-D995. https://doi.org/10.1093/nar/gks1193.
Sweeney TE, Haynes WA, Vallania F, Ioannidis JP, Khatri P. Methods to increase reproducibility in differential gene expression via meta-analysis. Nucleic Acids Res. 2017; 45:e1–e14. https://doi.org/10.1093/nar/gkw797.
Demšar J, Curk T, Erjavec A, Gorup C, Hocevar T, Milutinovic M, Možina M, Polajnar M, Toplak M, Starič A, Štajdohar A, Umek L, Žagar L, Žbontar J, Žitnik M, Zupan B. Orange: Data Mining Toolbox in Python. J Mach Learn Res. 2013; 14:2349–2353
Kanehisa M, Goto S, Furumichi M, Tanabe M, Hirakawa M. KEGG for representation and analysis of molecular networks involving diseases and drugs. Nucleic Acids Res. 2010; 38:D355-D360. https://doi.org/10.1093/nar/gkp896.
Xie Z, Bailey A, Kuleshov MV, Clarke DJB, Evangelista JE, Jenkins SL, Lachmann A, Wojciechowicz ML, Kropiwnicki E, Jagodnik KM, Jeon M, Ma'ayan A. Gene Set Knowledge Discovery with Enrichr Curr Protoc. 2021; 1:e90-e174. https://doi.org/10.1002/cpz1.90.
Shannon P, Markiel A, Ozier O, Baliga NS, Wang JT, Ramage D, Amin N, Schwikowski B, Ideker T. Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res. 2003; 13:2498–2504. https://doi.org/10.1101/gr.1239303.
Yu D, Lim J, Wang X, Liang F, Xiao G. Enhanced construction of gene regulatory networks using hub gene information. BMC Bioinformatics 2017; 18:186-206. https://doi.org/10.1186/s12859-017-1576-1.
Sander T, Freyss J, von Korff M, Rufener C. DataWarrior: an open-source program for chemistry aware data visualization and analysis. J Chem Inf Model. 2015; 55:460–473. https://doi.org/10.1021/ci500588j.
Mendez D, Gaulton A, Bento AP, Chambers J, De Veij M, Félix E, Magariños MP, Mosquera JF, Mutowo P, Nowotka M, Gordillo-Marañón M, Hunter F, Junco L, Mugumbate G, Rodriguez-Lopez M, Atkinson F, Bosc N, Radoux CJ, Segura-Cabrera A, Hersey A, Leach AR. ChEMBL: towards direct deposition of bioassay data. Nucleic Acids Res. 2019; 47:D930–D940. https://doi.org/10.1093/nar/gky1075.
Frimayanti N, Yam ML, Lee HB, Othman R, Zain SM, Rahman NA. Validation of quantitative structure-activity relationship (QSAR) model for photosensitizer activity prediction. Int J Mol Sci. 2011; 12:8626–8644. https://doi.org/10.3390/ijms12128626.
Sayers EW, Bolton EE, Brister JR, Canese K, Chan J, Comeau DC, Connor R, Funk K, Kelly C, Kim S, Madej T, Marchler-Bauer A, Lanczycki C, Lathrop S, Lu Z, Thibaud-Nissen F, Murphy T, Phan L, Skripchenko Y, Tse T, Wang J, Williams R, Trawick BW, Pruitt KD, Sherry ST. Database resources of the national center for biotechnology information. Nucleic Acids Res. 2022; 50:D20–D26. https://doi.org/10.1093/nar/gkab1112.
Tuccinardi T, Poli G, Romboli V, Giordano A, Martinelli A. Extensive consensus docking evaluation for ligand pose prediction and virtual screening studies. J Chem Inf Model. 2014; 54:2980–2986. https://doi.org/10.1021/ci500424n.
Molexus ApS. molegro virtual docker user manual. P. Baatrupsvej 41, DK-8300 Odder, Denmark: 2019.
Gabrielli AP, Manzardo AM, Butler MG. GeneAnalytics Pathways and Profiling of Shared Autism and Cancer Genes. Int J Mol Sci. 2019; 20(5):1166-1180 https://doi.org/10.3390/ijms20051166.
Indrayanto G, Putra GS, Suhud F. Validation of in-vitro bioassay methods: Application in herbal drug research. Profiles Drug Subst Excip Relat Methodol. 2021; 46:273–307. https://doi.org/10.1016/bs.podrm.2020.07.005.
Zou YF, Zhang SY, Li LW, Jing K, Xia L, Sun CX, Wu B. Hub genes for early diagnosis and therapy of adamantinomatous craniopharyngioma. Medicine 2022; 101:37-47. https://doi.org/10.1097/MD.0000000000030278.
Chen M, Pan J, Wang G. Identification and Functional Analysis of Hub Genes in Cell Cycle Pathway Linked to the Development of Lung Cancer with Non-Small Cells. Highlights Sci. Eng. Technol. 2023; 74:1501-1512.
Copps KD, White MF. Regulation of insulin sensitivity by serine/threonine phosphorylation of insulin receptor substrate proteins IRS1 and IRS2. Diabetologia. 2012; 55:2565–2582. https://doi.org/10.1007/s00125-012-2644-8.
Geering B, Cutillas PR, Vanhaesebroeck B. Regulation of class IA PI3Ks: is there a role for monomeric PI3K subunits? Biochem Soc Trans. 2007; 35:199–203. https://doi.org/10.1042/BST0350199.
Luo J, Cantley LC. The negative regulation of phosphoinositide 3-kinase signaling by p85 and it’s implication in cancer. Cell Cycle. 2005; 4:1309–1312. https://doi.org/10.4161/cc.4.10.2062.
Vallejo-Díaz J, Chagoyen M, Olazabal-Morán M, González-García A, Carrera AC. The Opposing Roles of PIK3R1/p85α and PIK3R2/p85β in Cancer. Trends Cancer. 2019; 5:233–244. https://doi.org/10.1016/j.trecan.2019.02.009.
Ma L, Murea M, Snipes JA, Marinelarena A, Krüger J, Hicks PJ, Langberg KA, Bostrom MA, Cooke JN, Suzuki D, Babazono T, Uzu T, Tang SC, Mondal AK, Sharma NK, Kobes S, Antinozzi PA, Davis M, Das SK, Rasouli N, Kern PA, Shores NJ, Rudel LL, Blüher M, Stumvoll M, Bowden DW, Maeda S, Parks JS, Kovacs P, Hanson RL, Baier LJ, Elbein SC, Freedman BI. An ACACB variant implicated in diabetic nephropathy associates with body mass index and gene expression in obese subjects. PLoS One. 2013; 8:e56193-e56203. https://doi.org/10.1371/journal.pone.0056193.
Millward CA, Desantis D, Hsieh CW, Heaney JD, Pisano S, Olswang Y, Reshef L, Beidelschies M, Puchowicz M, Croniger CM. Phosphoenolpyruvate carboxykinase (Pck1) helps regulate the triglyceride/fatty acid cycle and development of insulin resistance in mice. J Lipid Res. 2010; 51:1452–1463. https://doi.org/10.1194/jlr.M005363.
Onai N, Tsunokawa Y, Suda M, Watanabe N, Nakamura K, Sugimoto Y, Kobayashi Y. Inhibitory effects of bisbenzylisoquinoline alkaloids on induction of proinflammatory cytokines, interleukin-1 and tumor necrosis factor-alpha. Planta Med. 1995; 61:497–501. https://doi.org/10.1055/s-2006-959356.