Anti-Inflammatory and Analgesic Activities of Aqueous Extracts from Stigma maydis: In Silico and In Vivo Investigations
Main Article Content
Abstract
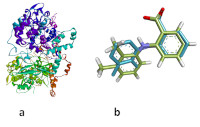
Chronic inflammation is a major global health concern, leading to diseases like cardiovascular disorders, cancer, diabetes, and kidney failure. The long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs) to manage inflammation is associated with adverse effects. The present study evaluated the anti-inflammatory and analgesic properties of an aqueous extract from Stigma maydis (SAE), a traditional herb known for its medicinal benefits. Aqueous extract was prepared from Stigma maydis and subjected to phytochemical screening. Physicochemical and pharmacokinetic properties of SAE were predicted using pkCSM and Swiss-ADME platforms. In silico molecular docking was performed on SAE's phytoconstituents. The anti-inflammatory activity of SAE was evaluated in rats using carrageenan-induced paw edema, with doses of 125, 250, and 500 mg/kg and mefenamic acid as a reference. Analgesic activity was assessed through the Randall-Selitto assay. The results revealed the presence of flavonoids, saponins, alkaloids, terpenoids, and phenolic compounds. In silico analysis identified several active constituents, such as pelargonidin and apigenidin, which exhibited a high binding affinity for cyclooxygenase-2, a key target for anti-inflammatory drugs. The extracts at doses of 125, 250, and 500 mg/kg significantly (p < 0.5) reduced paw edema, with inflammation percentages of 21.63, 22.64, and 24.69%, respectively, compared to the negative control group. The 500 mg/kg dose of SAE exhibited the most pronounced effects, although it was less potent than the positive control. The Result of the study revealed that Stigma maydis aqueous extract exhibited anti-inflammatory and analgesic properties with minimal side effects, warranting further research to understand its mechanisms of action and clinical applications.
Downloads
Article Details
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
How to Cite
References
1. Aksentijevich M, Lateef SS, Anzenberg P, Dey AK, Mehta NN. Chronic inflammation, cardiometabolic diseases and effects of treatment: psoriasis as a human model. Trends Cardiovasc Med. 2020; 30(8): 472-478. https://doi.org/10.1016/j.tcm.2019.11.001
2. Ronchetti S, Migliorati G, Delfino DV. Association of inflammatory mediators with pain perception. Biomed Pharmacother. 2017; 96: 1445-1452. https://doi.org/10.1016/j.biopha.2017.12.001
3. De la Cruz-Ahumada CJ, Topete-Reyes JF, Mena-Ramírez JP, Guzmán-Flores JM, Guzmán-González JI, Ramírez-De los Santos S. Inflammatory Determinants and Associated Morbidity in Hemodialysis Patients. J Pers Med. 2023; 13(9):1311. https://doi.org/10.3390%2Fjpm13091311
4. Bindu S, Mazumder S, Bandyopadhyay U. Non-steroidal anti-inflammatory drugs (NSAIDs) and organ damage: A current perspective. Biochem Pharmacol. 2020; 180: 114147. https://doi.org/10.1016%2Fj.bcp.2020.114147
5. Sohail R, Mathew M, Patel KK, Reddy SA, Haider Z, Naria M, Ayesha Habib A, Abdin ZU, Chaudhry WR, Akbar A. Effects of non-steroidal anti-inflammatory drugs (NSAIDs) and gastroprotective NSAIDs on the gastrointestinal tract: a narrative review. Cureus, 2023; 15(4): e37080. https://doi.org/10.7759%2Fcureus.37080
6. Hasanudin K, Hashim P, Mustafa S. Corn silk (Stigma maydis) in healthcare: a phytochemical and pharmacological review. Molecules. 2012; 17(8): 9697-9715. https://doi.org/10.3390/molecules17089697
7. Samee A, Amir RM, Ahmad A, Ali M, Afzal T, Zahoor Z, Asad M, Abbas M, Ali A, Fatima H. A nutraceutical approach towards corn silk. Int J Sci Res. 2023; 5(1): 093-097. https://doi.org/10.53430/ijsru.2023.5.1.0006
8. Lee CW, Seo JY, Kim SL, Lee J, Choi JW, Park YI. Corn silk maysin ameliorates obesity in vitro and in vivo via suppression of lipogenesis, differentiation, and function of adipocytes. Biomed Pharmacother. 2017; 93: 267-275. https://doi.org/10.1016/j.biopha.2017.06.039
9. Ryuk JA, Ko BS, Moon NR, Park S. Protection against neurological symptoms by consuming corn silk water extract in artery-occluded gerbils with reducing oxidative stress, inflammation, and post-stroke hyperglycemia through the gut-brain axis. Antioxidants. 2022; 11(1): 168. https://doi.org/10.3390/antiox11010168
10. Singh J, Inbaraj BS, Kaur S, Rasane P, Nanda V. Phytochemical analysis and characterization of corn silk (Zea mays, G5417). Agronomy. 2022; 12(4): 777. https://doi.org/10.3390/agronomy12040777
11. Chaves JO, De Souza MC, Da Silva LC, Lachos-Perez D, Torres-Mayanga PC, Machado APDF, Carneiro TF, Espinosa MV, Peredo AFG, Barbero GF, Rostagno M A. Extraction of flavonoids from natural sources using modern techniques. Front Chem. 2020; 8: 507887. https://doi.org/10.3389/fchem.2020.507887
12. Bitwell C, Indra SS, Luke C, Kakoma MK. A review of modern and conventional extraction techniques and their applications for extracting phytochemicals from plants. Sci Afr. 2023; 19: e01585. https://doi.org/10.1016/j.sciaf.2023.e01585
13. Dubale S, Kebebe D, Zeynudin A, Abdissa N, Suleman S. Phytochemical screening and antimicrobial activity evaluation of selected medicinal plants in Ethiopia. J Exp Pharmacol. 2023; 15: 51–62. https://doi.org/10.2147/JEP.S379805
14. Ortiz CLD, Completo GC, Nacario RC, Nellas RB. Potential inhibitors of galactofuranosyltransferase 2 (GlfT2): molecular docking, 3D-QSAR, and in silico ADMETox studies. Sci Rep. 2019; 9(1): 17096. https://doi.org/10.1038/s41598-019-52764-8
15. Falodun A, Okunrobo LO, Uzoamaka N. Phytochemical screening and anti-inflammatory evaluation of methanolic and aqueous extracts of Euphorbia heterophyla Linn (Euphorbiaceae). Afr J Biotechnol. 2006; 5(6): 529-531. https://doi.org/10.5897/AJB2006.000-5043
16. Purnomo Y, Tilaqza A. Analgesic and anti-inflammatory activities of Urena lobata L. leaf extracts. Indones J Pharm. 2022; 33(4): 566-574. https://doi.org/10.22146/ijp.2145
17. Rahman MM, Rahaman MS, Islam MR, Rahman F, Mithi FM, Alqahtani T, Almikhlafi MA, Alghamdi SQ, Alruwaili AS, Hossain MS, Ahmed M, Das R, Emran TB, Uddin MS. Role of phenolic compounds in human disease: current knowledge and future prospects. Molecules. 2021; 27(1): 233. https://doi.org/10.3390%2Fmolecules27010233
18. Roy A, Khan A, Ahmad I, Alghamdi S, Rajab BS, Babalghith AO, Alshahrani MY, Islam S, Islam MR. Flavonoids a bioactive compound from medicinal plants and its therapeutic applications. Biomed Res Int. 2022; (1): 5445291. https://doi.org/10.1155%2F2022%2F5445291
19. Heinrich M, Mah J, Amirkia V. Alkaloids used as medicines: Structural phytochemistry meets biodiversity—An update and forward look. Molecules. 2021; 26(7): 1836. https://doi.org/10.3390%2Fmolecules26071836
20. Timilsena YP, Phosanam A, Stockmann R. Perspectives on saponins: food functionality and applications. Int J Mol Sci. 2023; 24(17): 13538. https://doi.org/10.3390/ijms241713538
21. Chen X, Li H, Tian L, Li Q, Luo J, Zhang Y. Analysis of the physicochemical properties of acaricides based on Lipinski's rule of five. J Comput Biol. 2020; 27(9): 1397-1406. https://doi.org/10.1089/cmb.2019.0323
22. Purnomo Y, Tilaqza A, Zubair MS, Mustopa AZ. Immunopotentiator of terpenoid from Hibiscus tiliaceus leaf fraction as candidate of vaccine adjuvants with in silico study. S Afr J Bot. 2024; 172: 19-30. https://doi.org/10.1016/j.sajb.2024.06.051
23. Purnomo Y, Tilaqza A. Inhibitory Potential of Pulutan (Urena lobata) Leaf Extract on Inducible Nitric Oxide Synthase as Anti-inflammatory Agent: In Vitro and In Silico Approaches. Trop J Nat Prod Res. 2024; 8(8): 8195 – 8201 .https://doi.org/10.26538/tjnpr/v8i8.41
24. Lipinski CA, Lombardo F, Dominy BW, Feeney PJ. Experimental and computational approaches to estimate solubility and permeability in drug discovery and development settings. Adv Drug Deliv Rev. 2012; 64: 4-17. https://doi.org/10.1016/j.addr.2012.09.019
25. Juvale IIA, Hamid AAA, Abd Halim KB, Has ATC. P-glycoprotein: New insights into structure, physiological function, regulation and alterations in disease. Heliyon. 2022; 8(6): e09777. https://doi.org/10.1016/j.heliyon.2022.e09777
26. Geldenhuys WJ, Mohammad AS, Adkins CE, Lockman PR. Molecular determinants of blood–brain barrier permeation. Ther Deliv. 2015; 6(8): 961-971. https://doi.org/10.4155/tde.15.32
27. Chandrasekaran B, Abed SN, Al-Attraqchi O, Kuche K, Tekade R. Computer-aided prediction of pharmacokinetic (ADMET) properties. In Dosage form design parameters. Academic Press; 2018. 731-755p. https://doi.org/10.1016/B978-0-12-814421-3.00021-X
28. Zuo HL, Huang HY, Lin YCD, Cai XX, Kong XJ, Luo DL, Zhou YH, Huang HD. Enzyme Activity of Natural Products on Cytochrome P450. Molecules. 2022; 27(2): 515. https://doi.org/10.3390/molecules27020515
29. Ahmad I, Kuznetsov AE, Pirzada AS, Alsharif KF, Daglia M, And Khan H. Computational pharmacology and computational chemistry of 4-hydroxyisoleucine: Physicochemical, pharmacokinetic, and DFT-based approaches. Front Chem. 2023; 11: 1145974. https://doi.org/10.3389/fchem.2023.1145974
30. Du X, Li Y, Xia YL, Ai SM, Liang J, Sang P, Ji XL, Liu SQ. Insights into protein–ligand interactions: mechanisms, models, and methods. Int J Mol Sci. 2016; 17(2): 144. https://doi.org/10.3390/ijms17020144
31. Lu W, Zhang J, Huang W, Zhang Z, Jia X, Wang Z, Shi L, Li C, Wolynes PG, Zheng, S. Dynamic Bind: Predicting ligand-specific protein-ligand complex structure with a deep equivariant generative model. Nat Commun. 2024; 15(1): 1071. https://doi.org/10.1038/s41467-024-45461-2
32. Purnomo Y, Wahyuningsih D, Tilaqza A. Anti-inflammatory potency of pulutan (Urena lobata) leaf extract and its fractions by protein denaturation inhibition assay. Res J Pharm Technol. 2023; 16(11): 5406-5409. https://doi.org/10.52711/0974-360X.2023.00875
33. Al-Khayri JM, Sahana GR, Nagella P, Joseph BV, Alessa FM, Al-Mssallem MQ. Flavonoids as potential anti-inflammatory molecules: A review. Molecules. 2022; 27(9): 2901. https://doi.org/10.3390/molecules27092901
34. Wu YL, Han F, Luan SS, Ai R, Zhang P, Li H, Chen LX. Triterpenoids from Ganoderma lucidum and their potential anti-inflammatory effects. J Agric Food Chem. 2019; 67(18): 5147-5158. https://doi.org/10.1021/acs.jafc.9b01195
35. Cui J, Jia J. Natural COX-2 inhibitors as promising anti-inflammatory agents: an update. Curr Med Chem. 2021; 28(18): 3622-3646. https://doi.org/10.2174/0929867327999200917150939
36. Cui Y, Jiang L, Yu R, Shao Y, Mei L, Tao Y. β-carboline alkaloids attenuate bleomycin induced pulmonary fibrosis in mice through inhibiting NF-kb/p65 phosphorylation and epithelial-mesenchymal transition. J Ethnopharmacol. 2019; 243: 112096. https://doi.org/10.1016/j.jep.2019.112096
37. Zhou Y, Zhong B, Min X, Hou Y, Lin L, Wu Q, Shi J, Chen X. Therapeutic potential of isobavachalcone, a natural flavonoid, in murine experimental colitis by inhibiting NF‐κβ p65. Phytother Res. 2021; 35(10): 5861-5870. https://doi.org/10.1002/ptr.7246
38. Chen M, Qin Y, Ma H, Zheng X, Zhou R, Sun S, Huang Y, Duan Q, Liu W, Wu P, Xu X, Sheng Z, Zhang K, Li D. Downregulating NF-κβ signalling pathway with triterpenoids for attenuating inflammation: in vitro and in vivo studies. Food Funct. 2019; 10(8): 5080-5090. https://doi.org/10.1002/ptr.7246
39. Zhang L, Ravipati AS, Koyyalamudi SR, Jeong SC, Reddy N, Smith PT, Bartlett J, Shanmugam K, Münch G, Wu MJ. Antioxidant and anti-inflammatory activities of selected medicinal plants containing phenolic and flavonoid compounds. J Agric Food Chem. 2011; 59(23): 12361-12367. https://doi.org/10.1021/jf203146e
40. Lopez Corona AV, Valencia-Espinosa I, González-Sánchez FA, Sánchez-López AL, Garcia-Amezquita LE, Garcia-Varela R. Antioxidant, anti-inflammatory and cytotoxic activity of phenolic compound family extracted from raspberries (Rubus idaeus): A general review. Antioxidants. 2022; 11(6): 1192. https://doi.org/10.3390/antiox11061192
41. Silva-Correa CR, Campos-Reyna JL, Villarreal-La TVE, Calderón-Peña AA, Blas MVG, Aspajo-Villalaz CL, Razco JLC, Guarniz WAS, Guerrero-Espino LM, Julio H. Potential activity of medicinal plants as pain modulators: a review. Phcog J. 2021; 13(1): 248-263. http://dx.doi.org/10.5530/pj.2021.13.35
42. Wang TX, Wu GJ, Jiang JG. Natural products with analgesic effects from herbs and nutraceuticals used in traditional Chinese medicines. Curr Mol Med. 2020; 20(6): 461-483. https://doi.org/10.2174/1566524019666191205111937
43. Liu W, Cui X, Zhong Y, Ma R, Liu B, Xia Y. Phenolic metabolites as therapeutic in inflammation and neoplasms: Molecular pathways explaining their efficacy. Pharmacol Res. 2023; 193: 106812. https://doi.org/10.1016/j.phrs.2023.106812
44. Nurrosyidah IH, Mertaniasih NM, Isnaeni. The effect of red passion fruit (Passiflora edulis Sims.) fermentation time on its activity against Extended Strain Methicillin-Resistant (ESBL) Escherichia coli and Methicillin-Resistant Staphylococcus aureus (MRSA). J Basic Clin Physiol Pharmaco. 2021; 32(4): 723-727. https://doi.org/10.1515/jbcpp-2020-0408