Gas Chromatography-Mass Spectrometry Analysis and Antimalarial Activity of Salix ledermannii Ethanol Leaves Extracts
Main Article Content
Abstract
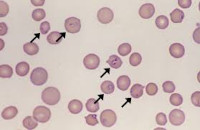
Although malaria is curable, it remains the leading cause of mortality in Nigeria. Eliminating malaria is a pressing concern due to the challenge of drug-resistant Plasmodium parasites. Therefore, there is an urgent need for antimalarial agents that are affordable, safe, and effective against drug-resistant strains. The antimalarial potential of Salix ledermannii ethanol leaf extracts and their effect on PCV and haemoglobin levels, as well as the phytochemical compositions of the extract, were evaluated in this study using Plasmodium berghei infected mice as models. 0.2 ml Distilled water (Dw) was used as the negative control, while 5 mg/kg chloroquine and 1.2 mg/kg pyrimethamine served as the positive control. The phytochemical composition was analysed using standard chemical tests and GC-Ms techniques. Compared to the negative control, S. ledermannii showed significant chemo-suppression at 100 mg (44.38 %) and 300 mg/kg (46.75 %). Also, 5 mg/kg-chloroquine and treatment at 300 mg/kg significantly inhibited parasitaemia compared to the control group in the curative test model (p<0.05). The prophylactic test did not differ significantly (p>0.05) across treatment groups. The crude extract contained alkaloids, tannins, steroids, terpenes, anthraquinones, phenols, and saponins, and GC-Ms analysis revealed forty-three (43) known compounds, with benzoic acid (27.21%), phenol (15.22%), β-D-Glucopyranose (12.29%), Salicylalcohol (11.88%), 1-Butanol, 3-methyl (6.93%), Catechol (6.35%) and -ethyl-5,6-dihydo-2H-pyran-2-one (5.48%) having the highest concentrations. S. ledermannii poses no adverse effect on PCV and H.B. levels of treated mice and exhibits significant antimalarial properties. Thus, this plant can serve as a novel lead for compounds in the next-generation antimalarial drugs.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
World Health Organization. World Health Statistics 2020. Geneva: World Health Organization; 2020. https://apps.who.int/iris/handle/10665/11273819082021/9:09
Okell LC, Bousema T. The importance of malaria parasite density in subcontracting malaria elimination. Trends Parasitol. 2020; 36(1):33-44.
Trampuz A, Jereb M, Muzlovic I, Prabhu RM. Clinical review: Severe malaria. Crit Care. 2003;7(4):315-523.
Singh S, Singh R. Protozoal infections: A review on the recent advances and future direction. J Vector Borne Dis. 2022; 59(2):1-12.
Soniran OT, Idowu OA, Ajayi OL, Olubi IC. Comparative Study on the Effects of Chloroquine and Artesunate on Histopathological Damages Caused by Plasmodium berghei in Four Vital Organs of Infected Albino Mice. Malar Res Treat. 2012; 2012:960758
Bhattacharya S, Chakraborty S. Malaria: An overview on the recent advances and future challenges. J Med Microbiol Immunol. 2022;11(1) :1-12.
Ellis RA, Gould SJ. Salix (Willow) identification guide for the northeastern United States. Cambridge, MA: Harvard University Press; 2020.
Zhang M, Chen L, Wang H. Molecular phylogeny and biogeography of the genus Salix (Salicaceae) in Asia. J Plant Syst Evol. 2022 ;307(1-2) :1-12.
Tawfeek N, Mahmoud MF, Hamdan DI, Sobeh M, Farrag N, Wink M, El-Shazly AM. Phytochemistry, Pharmacology and Medicinal Uses of Plants of the Genus Salix: An Updated Review. Front Pharmacol. 2021; 12:593856.
Evbuomwan SA, Omotosho OE, Akinola OO. A Mini Review on Some Known Medicinal Uses of Tridax Procumbens. Trop J Nat Prod Res. 2023; 7(8):3573-3584.
Uma B, Prabhakar K, Rajendran S, Lakshmi SY. Studies on GC/MS spectroscopic analysis of some bioactive antimicrobial compounds from Cinnamomum zeylanicum. J Med Plants. 2009; 8(31):125–131.
Gebrehiwot T, Birhane E, Gebrehiwot G. Phytochemical screening and in vivo antimalarial activity of two traditionally used medicinal plants of Afar region, Ethiopia, against Plasmodium berghei in Swiss Albino mice. J Ethnopharmacol. 2019 ;231 :141-148.
Traisathit R, Sangdee A, Wongpakam K, Sedlak S, Kanjanasirirat P, Borwornpinyo S, Thita T, Patrapuvich R, Seephonkai P. Antioxidant, Antibacterial and Antiplasmodial Activities of Galactogogue Plant Extracts.Trop J Nat Prod Res. 2021; 5(4):698-706.
Jimoh AA, Maiha BB, Chindo BA, Ejiofor JI, Ehinmidu JO, Atang DA, Azi JY. In vitro Antiplasmodial Activity of Methanol Stem Extract of Costusafer Ker Gawl.(Costaceae) and its Residual Aqueous Fraction Against Some Drug-sensitive and drug-resistant Plasmodium falciparum Strains.Trop J Nat Prod Res. 2019;3(5):162-169
Tesfahuneygn G, Gebreegziabher Z. Phytochemical screening and ethnobotanical study of medicinal plants used in Ethiopian traditional medicine. J Pharm Pharmacol. 2019;71(9):1440-1448.
Hope O, Bright IE, Alagbonsi AI. GC-MS biocomponents characterisation and antibacterial potency of ethanol crude extracts of Camellia sinensis. SAGE Open Med. 2022;10:16859.
Lorke D. A new approach to practical acute toxicity testing. Arch Toxicol. 1983;54:275-287.
Dawet A, Yakubu DP, Wunnang NN, Mwansat GS. Invivo Antimalarial Activity of Stem Bark of Dry Zone Cedar Pseudocedrela kotschyi (Mellaceae) in Mice. Eur J Med Plants. 2014 ;4(3) :342-352.
Dawet A, Stephen MD. The Antimalarial Activity of the Crude Leaf Extract of Pseudocedrela kotschyi in Plasmodium berghei berghei Infected Mice. Afr J Nat Sci. 2014;17:19-27.
Uzor PF, Onyishi CK, Omaliko AP, Nworgu SA, Ugwu OH, Nwodo NJ. Study of the Antimalarial Activity of the Leaf Extracts and Fractions of Persea americana and Dacryodes edulis and Their HPLC Analysis. Evid Based Complement Alternat Med. 2021;2021:5218294
Kabiru AY, Abdulkadir, Gbodi AT, Bello UM, Makun HA, Amah DJ, Ogbadoyi EO. Evaluation of hematological changes in Plasmodium-berghei-infected mice administered with aqueous extract of Phyllantus amarus. Pak J Biol Sci. 2013 ;16 :510-516.
Suharsanti R, Astuti P, Yuniarti N, Wahyuono S. Review ofIsolation Methods, Chemical Composition and Biological Activities of Curcuma aeruginosa Roxb Rizhome. Trop J Nat Prod Res. 2022 ; 6(10):1538-1546.
Olajide IA, Oluwatosin OA, Oladosu IA. Qualitative phytochemical analysis of some selected medicinal plants in Nigeria. J Pharmacogn Phytochem. 2021 ;10(2) :108-116.
Falodun A, Erharuyi O, Imieje V, Ahomafor J, Akunyuli C, Jacobs M, Khan S, Hamann MT, Langer P. In vitro evaluation of aliphatic fatty alcohol metabolites of Persea americana seed as potential antimalarial and antimicrobial agents. Niger J Biotechnol. 2014; 27:1-7.
Muhaimin M, Latifah N, Chaerunisaa AY, Subarnas A, Susilawati Y, Hirzan R. Antiplasmodial Activity of Ethanol Extract of Sonneratia alba Leaves. Trop J Nat Prod Res. 2024; 8(4):6884-6890.
Haruna Y, Kwanashie HO, Anuka JA, Atawodi SE, Hussaini IM. In vivo antimalarial activity of methanol root extract of Securidaca long pedunculate in mice infected with Plasmodium berghei. Int J Mod Biol Med. 2013 ;3(1):7-16.
Alli LA, Adesokon AN, Salawu OA, Akanji MA, Tijani AY. Antiplasmodial activity of aqueous root extract of Acacia nilotica. Afr J Biochem Res. 2011; 5(7):214-219.
Bantie L, Assefa S, Teklehaimanot T, Engidawork E. In vivo antimalarial activity of the crude leaf extract and solvent fractions of Croton macrostachyus Hocsht. (Euphorbiaceae) against Plasmodium berghei in mice. B.M.C. Complement Altern Med. 2014;14:79.
Abosi AO, Raseroka BH. Invivo antimalarial activity of Vernonia amygdalina. Br J Biomed Sci. 2003;60(20):89-91.
Mbah CC, Akuodor AC, Anyalewechi NA, Iwuanyanwu TC, Osunkwo UA. In vivo, antiplasmodial activities of aqueous extract of Bridelia ferruginea stem bark against Plasmodium berghei berghei in mice. Pharmaceut. Biol. 2012; 50: 188-194
Oghogho UI, Ekugum E, Ogbeide OK, Idagan MI, Uadia JO, Falodun A.Phytochemical Assessment, Anti-inflammatory and Antimalarial Activities of Beta vulgaris (Chenopodiaceae) Root Extract. Trop J Phytochem Pharm Sci. 2022; 1(1):3-8.
Etkin NL. Antimalarial plants used by Hausa in Northern Nigeria. Trop Doct. 1997; 27:12-16.
Kirby GC, O'Neill MJ, Phillipson JD, Warhurst DC. In vitro studies on the mode of action of quassinoids with activity against chloroquine-resistant Plasmodium falciparum. Biochem Pharmacol. 1989; 38(24):4367-474.
Akuodor GC, Idris-Usman M, Anyalewechi N, Odo E, Ugwu C,T, Akpan JL, Gwotmut MD, Osunkwo, UA. In vivo Antimalarial Activity of Ethanol Leaf Extract of Verbena hastata Against Plasmodium berghei berghei in Mice. J Herb Med Toxicol. 2010 ;4(2) :17-23.
Lathia TB, Joshi R. Can haematological parameters discriminate malaria from non-malarious acute febrile illness in the tropics? Indian J Med Sci. 2004;58(6):239-244.