Pattern of Haematological Indices of Wistar Rats Administered Antiretroviral Therapy Singly or in Combination with Ascorbic Acid and α-Tocopherol
Main Article Content
Abstract
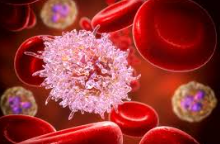
Antiretroviral therapy use in the treatment of HIV/AIDS, has previously been linked to anaemia or a decrease in haematologic performance. Given that HIV/AIDS has a significant impact on immune responses, using antioxidants in the treatment of these disease may improve immunological outcomes, as evidenced by haematologic indices. This investigation sought to ascertain the haematological response of Wistar arts treated orally with Lamivudine and Zidovudine along with Vitamins C and E. For 90 days, Wistar rats were given Zidovudine and Lamivodine orally along with vitamin C and E supplements. The rats were divided into groups: one group received Zidovudine and Lamivudine orally at a dose of 15 mg Zidovudine/kg/body and 7.5 mg Lamivudine/kg BW. Vitamin E was also administered at 25 IU/kg BW; the same dose was administered for Vitamin C. The other group received a combination of the antiretroviral drug (ARD) and an antioxidant. The last (or control) group received distilled water at 10ml/kg. At the end of the treatment , the Wistar rats were humanly sacrificed and whole blood collected into Ethylene Diamine tetraacetic acid containers for analysis of haematological indices. The effects of the antiretroviral therapy on red blood indices varied with the ARD administered; there was a significant increase in haematocrit levels in Lamivudine-treated Wistar rats (p<0.05). The results also revealed that lymphocyte concentration was more likely to be related with Lamivudine+Vitamin E treatment than with Lamivudine administration alone. Similarly, the combination of Zidovudine and Vitamin C was more likely to impact platelet count concentrations than Zidovudine alone.
Downloads
Article Details
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
How to Cite
References
Dadkhah M, Matin S, Safarzadeh E, Rezaei N, Negaresh M, Salehzadeh H, Matin S, Sharifiazar A, Abazari M. Hematological Parameters as Diagnostic Factors: Correlation with Severity of COVID-19. Acta Biomed. 2022;93(2):e2022061. doi: 10.23750/abm.v93i2.12320.
Takami A. Molecular Immunology in Hematological Disorders. Int J Mol Sci. 2022;23(17):9584. doi: 10.3390/ijms23179584.
McLean E, Cogswell M, Egli I, Wojdyla D, De Benoist B. Worldwide prevalence of anaemia WHO vitamin and mineral nutrition information system 1993–2005. Public Health Nutr 2009; 12(4):444–454
Assefa M, Abegaz WE, Shewamare A, Medhin G, Belay M. Prevalence and correlates of anemia among HIV infected patients on highly active anti-retroviral therapy at Zewditu Memorial Hospital Ethiopia. BMC Hematol 2015; 15(1):6
Wang W, Dong Z, Zhang J, Zhou X, Wei X, Cheng F, Li B, Zhang J. Acute and Subacute Toxicity Assessment of Oxyclozanide in Wistar Rats. Front Vet Sci 2019; 6:294 doi: 103389/fvets201900294
Karber G. Reihenversucbe. Arch Exper Pathol Pharmacol 1991; 162: 480-483.
Muhammad NO, Akolade JO, Usman LA, Oloyede OB. Haematological parameters of alloxan-induced diabetic rats treated with leaf essential oil of Hoslundia opposita (Vahl). EXCLI J. 2012;11:670-6.
Belperio PS, Rhew DC. Prevalence and outcomes of anemia in individuals with human immunodeficiency virus: a systematic review of the literature. Am J Med 2004; 116(7):27–43.
Calis JC, van Hensbroek MB, de Haan RJ, Moons P, Brabian BJ, Bates I. HIV-associated anemia in children: systemic review from global perspective. AIDS 2008; 22(10):1099–1112 doi: 101097/QAD0b013e3282fa759f
Kibaru EG, Nduati R, Wamalwa D, Kariuki N. Impact of highly active antiretroviral therapy on hematological indices among HIV-1 infected children at Kenyatta National Hospital-Kenya: retrospective study. AIDS Research and Therapy 2015; 12 26 https://doiorg/101186/s12981-015-0069-4
Ogeyemhe BE, Amaechi RA, Ekpruke CD, Airiagbonbu BO, Odigie EB. comparative benefits of cocos nucifera l. husk, milk and shell extracts on body weight changes and haematological indices in male Rats: Trop J Nat Prod Res 2020; 21: 4(8):455-62. doi.org/10.26538/tjnpr/v4i8.22.
John MA, Rhemtula YA, Menezes CN, Grobusch MP. Lamivudine-induced red cell aplasia. J. of Med Micro 2008; 57(Pt 8) 1032–1035 https://doiorg/101099/jmm047782-0