Anticancer and Antioxidant Effects of Sitagliptin and Linagliptin against Lung Cancer Cell Lines (an In vitro Study)
Main Article Content
Abstract
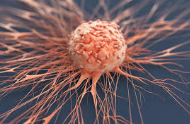
Lung cancer has the highest global fatality rate of all cancers, and most existing therapies have a wide range of toxic effects. This necessitates searching for new medications with potential anticancer properties and a better safety profile against normal cells. Dipeptidyl peptidase-4 (DPP4) inhibitors have recently shown anticancer efficacy in various malignancies such as colorectal, prostate, and renal cancer. Therefore, this study investigated the anticancer activity of sitagliptin (SITA) and linagliptin (LINA) against the lung cancer cell line A549 alone and in combination with cisplatin (CP). A549 cells were divided into six groups: control (untreated cells), CP-treated cells, SITA-treated cells, LINA-treated cells, CP plus SITA-treated cells (ratio 1:1), and CP plus LINA-treated cells (ratio 1:1). After 72 hours of incubation, a 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl-2H-tetrazolium bromide (MTT) test was used to determine cell viability and the concentration of 50% inhibition for cell viability (IC50) for each group. A549 cells were later seeded in six flasks and treated with the resulting IC50; cell pellets were collected and lysed to determine the malondialdehyde (MDA) level using ELISA kits. SITA and LINA therapy dramatically reduced A549 cell viability compared to the control (P < 0.0001), with results comparable to CP. When SITA and LINA were combined with CP, they demonstrated significantly higher anticancer efficacy than when used alone. Notably, both medicines lowered MDA levels when taken alone or in combination with CP. SITA and LINA showed promising anticancer and antioxidant activity against A549 cells. This may indicate a potential synergistic anticancer effect with CP.
Downloads
Article Details
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
How to Cite
References
Al-Tariahi KMJ, Hameed WS, Abdul DH, Saheb AM. Evaluation of CA125 as a marker in patients with lung carcinoma. 2015.
Riihimäki M, Hemminki A, Fallah M, Thomsen H, Sundquist K, Sundquist J, Hemminki K. Metastatic sites and survival in lung cancer. Lung Cancer. 2014;86(1):78-84.
Merabishvili VM, Arseniev AI, Tarkov SA, Barchuk AA, Shcherbakov AМ, Demin E V, Merabishvili EN. Lung cancer morbidity and mortality. Sib J Oncol. 2018;17(6):15-26.
Benitez Majano S, Ellis L, Rachet B. Epidemiology of Lung Cancer. In: Encyclopedia of Respiratory Medicine (Second Edition). 2022 Jan 1; 4:663-72.
Thandra KC, Barsouk A, Saginala K, Aluru JS, Barsouk A. Epidemiology of lung cancer. Współczesna Onkol. 2021;25(1):45-52.
Schabath MB, Cote ML. Cancer progress and priorities: lung cancer. Cancer Epidemiol Biomarkers Prev. 2019;28(10):1563-79.
Reck M, Rabe KF. Precision diagnosis and treatment for advanced non–non-small-cell lung cancer. N Engl J Med. 2017;377(9):849-61.
Brown A, Kumar S, Tchounwou PB. Cisplatin-Based Chemotherapy of Human Cancers. J Cancer Sci Ther. 2019;11.
Tchounwou PB, Dasari S, Noubissi FK, Ray P, Kumar S. Advances in our understanding of the molecular mechanisms of action of Cisplatin in cancer therapy. J Exp Pharmacol. 2021:303-28.
Dasari S, Tchounwou PB. Cisplatin in cancer therapy: molecular mechanisms of action. Eur J Pharmacol. 2014; 740:364-78.
Aldossary SA. Review on pharmacology of Cisplatin: clinical use, toxicity and mechanism of resistance of Cisplatin. Biomed Pharmacol J. 2019;12(1):7-15.
Almagthali AG, Alkhaldi EH, Alzahrani AS, Alghamdi AK, Alghamdi WY, Kabel AM. Dipeptidyl peptidase-4 inhibitors: Anti-diabetic drugs with potential effects on cancer. Diabetes Metab Syndr Clin Res Rev. 2019;13(1):36-43.
Wilson AL, Moffitt LR, Wilson KL, Bilandzic M, Wright MD, Gorrell MD, Oehler MK, Plebanski M, Stephens AN. DPP4 inhibitor sitagliptin enhances lymphocyte recruitment and prolongs survival in a syngeneic ovarian cancer mouse model. Cancers (Basel). 2021;13(3):487.
Gilbert MP, Pratley RE. GLP-1 analogs and DPP-4 inhibitors in type 2 diabetes therapy: a review of head-to-head clinical trials. Front Endocrinol (Lausanne). 2020; 11:178.
Holst JJ, Gasbjerg LS, Rosenkilde MM. The role of incretins on insulin function and glucose homeostasis. Endocrinology. 2021;162(7): bqab065.
Raz I, Hanefeld M, Xu L, Caria C, Williams-Herman D, Khatami H. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor sitagliptin as monotherapy in patients with type 2 diabetes mellitus. Diabetologia. 2006; 49:2564-71.
Pro B, Dang NH. CD26/dipeptidyl peptidase IV and its role in cancer. Histol Histopathol. 2004 Oct;19(4):1345-51.
Havre PA, Abe M, Urasaki Y, Ohnuma K, Morimoto C, Dang NH. The role of CD26/dipeptidyl peptidase IV in cancer. Front Biosci. 2008; 13:1634-45.
Femia AP, Raimondi L, Maglieri G, Lodovici M, Mannucci E, Caderni G. Long‐term treatment with Sitagliptin, a dipeptidyl peptidase‐4 inhibitor, reduces colon carcinogenesis and reactive oxygen species in 1, 2‐dimethylhydrazine‐induced rats. Int J Cancer. 2013;133(10):2498-503.
Lam CSC, Cheung AHK, Wong SKM, Wan TMH, Ng L, Chow AKM, Cheng NS, Pak RC, Li HS, Man JH, Yau TC. Prognostic significance of CD26 in patients with colorectal cancer. PLoS One. 2014;9(5): e98582.
Javidroozi M, Zucker S, Chen WT. Plasma seprase and DPP4 levels as markers of disease and prognosis in cancer. Dis Markers. 2012;32(5):309-20.
Boccardi V, Marano L, Rossetti RRA, Rizzo MR, di Martino N, Paolisso G. Serum CD26 levels in patients with gastric cancer: a novel potential diagnostic marker. BMC Cancer. 2015;15(1):1-6.
Amritha CA, Kumaravelu P, Chellathai DD. Evaluation of Anticancer Effects of DPP-4 Inhibitors in Colon Cancer- An Invitro Study. J Clin Diagn Res. 2015 9(12): FC14-6.
Tseng CH. Sitagliptin may reduce breast cancer risk in women with type 2 diabetes. Clin Breast Cancer. 2017;17(3):211-8.
Tseng CH. Sitagliptin may reduce prostate cancer risk in male patients with type 2 diabetes. Oncotarget. 2017;8(12):19057.
Kabel AM, Atef A, Estfanous RS. Ameliorative potential of Sitagliptin and/or resveratrol on experimentally-induced clear cell renal cell carcinoma. Biomed Pharmacother. 2017; 97:667-74.
Bishnoi R, Hong Y, Shah C, Ali A, Skelton IV WP, Huo J, Dang NH, Dang LH. Dipeptidyl peptidase 4 inhibitors as novel agents in improving survival in diabetic patients with colorectal cancer and lung cancer: A Surveillance Epidemiology and Endpoint Research Medicare study. Cancer Med. 2019;8(8):3918-27.
Salama MM, Zaghloul RA, Khalil RM, El-Shishtawy MM. Sitagliptin Potentiates the Anti-Neoplastic Activity of Doxorubicin in Experimentally-Induced Mammary Adenocarcinoma in Mice: Implication of Oxidative Stress, Inflammation, Angiogenesis, and Apoptosis. Sci Pharm. 2022;90(3).
Giard DJ, Aaronson SA, Todaro GJ, Arnstein P, Kersey JH, Dosik H, Parks WP. In Vitro Cultivation of Human Tumors: Establishment of Cell Lines Derived from a Series of Solid Tumors2. JNCI J Natl Cancer Inst. 1973;51(5):1417-23.
Van Meerloo J, Kaspers GJL, Cloos J. Cell sensitivity assays: the MTT assay. In: Cancer cell Culture methods Protocols. 2011:237-45.
Oiseoghaede JO, Oyawaluja AA, Sowemimo AA, Odukoya OA, Che CT. Antiproliferative potential of ethanol leaf extract of Motandra guineensis (Thonn.) A. DC. (Apocynaceae) against human melanoma and ovarian cancer cells. Trop J Nat Prod Res. 2024;8(3 SE-Articles):6700-4.
Bukowski K, Kciuk M, Kontek R. Mechanisms of multidrug resistance in cancer chemotherapy. Int J Mol Sci. 2020;21(9):3233.
Nakashima T, Nagano S, Setoguchi T, Sasaki H, Saitoh Y, Maeda S, Komiya S, Taniguchi N. Tranilast enhances the effect of anticancer agents in osteosarcoma. Oncol Rep. 2019;42(1):176-88.
Jin X, Wei Y, Liu Y, Lu X, Ding F, Wang J, Yang S. Resveratrol promotes sensitization to Doxorubicin by inhibiting epithelial‐mesenchymal transition and modulating the SIRT1/β‐catenin signaling pathway in breast cancer. Cancer Med. 2019;8(3):1246-57.
Jung Y, Lippard SJ. Direct cellular responses to platinum-induced DNA damage. Chem Rev. 2007;107(5):1387-407.
Qi L, Luo Q, Zhang Y, Jia F, Zhao Y, Wang F. Advances in toxicological research of the anticancer drug cisplatin. Chem Res Toxicol. 2019;32(8):1469-86.
Jang JH, Janker F, De Meester I, Arni S, Borgeaud N, Yamada Y, Gil Bazo I, Weder W, Jungraithmayr W. The CD26/DPP4-inhibitor vildagliptin suppresses lung cancer growth via macrophage-mediated NK cell activity. Carcinogenesis. 2019;40(2):324-34.
Varela‐Calviño R, Rodríguez‐Quiroga M, Dias Carvalho P, Martins F, Serra‐Roma A, Vázquez‐Iglesias L, Paez de la Cadena M, Velho S, Cordero OJ. The mechanism of sitagliptin inhibition of colorectal cancer cell lines’ metastatic functionalities. IUBMB Life. 2021;73(5):761-73.
Li Y, Li Y, Li D, Li K, Quan Z, Wang Z, Sun Z. Repositioning of Hypoglycemic Drug Linagliptin for Cancer Treatment. Front Pharmacal. 2020; 11:187.
Mani RJ, Anand M, Agarwal K, Tiwari A, Amanur Rahman Hashmi Q, Vikram Singh T, Nongdam P, Katare DP, Potshangabam AM. A Systematic Review of Molecular Pathway Analysis of Drugs for Potential Use in Liver Cancer Treatment. Drugs Drug Candidates. 2023;2(2):210-31.
Kosowska A, Garczorz W, Kłych-Ratuszny A, Aghdam MRF, Kimsa-Furdzik M, Simka-Lampa K, Francuz T. Sitagliptin modulates the response of ovarian cancer cells to chemotherapeutic agents. Int J Mol Sci. 2020;21(23):1-13.
Pethanasamy M, Suchitra MR, Sivasankaran SM, Surya S, Elanchezhiyan C, Thara JM. In vitro Evaluation of the Antioxidant and Anticancer Activities of Chlorogenic Acid on Human Colon Cancer (HT-29) Cells. Trop J Nat Prod Res. 2024;8(3 SE-Articles):6582-8.
Klaunig JE. Oxidative stress and cancer. Curr Pharm Des. 2018;24(40):4771-8.
Hayes JD, Dinkova-Kostova AT, Tew KD. Oxidative stress in cancer. Cancer Cell. 2020;38(2):167-97.
Ghosh S. Cisplatin: The first metal-based anticancer drug. Bioorg Chem. 2019; 88:102925.
Shaloam RD. Preclinical Assessment of Low Doses of Cisplatin in the Management of Acute Promyelocytic Leukemia. Int J Cancer Res Mol Mech. 2015;1.
Soni H, Kaminski D, Gangaraju R, Adebiyi A. Cisplatin-induced oxidative stress stimulates renal Fas ligand shedding. Ren Fail. 2018;40(1):314-22.
ElGamal RZ, Tadros MG, Menze ET. Linagliptin counteracts rotenone’s toxicity in a non-diabetic rat model of Parkinson’s disease: Insights into the neuroprotective roles of DJ-1, SIRT-1/Nrf-2, and implications of HIF1-α. Eur J Pharmacol. 2023 Feb 15; 941:175498.
Çadirci K, Türkez H, Özdemir Ö. The in vitro cytotoxicity, genotoxicity, and oxidative damage potential of the oral dipeptidyl peptidase-4 inhibitor, linagliptin, on cultured human mononuclear blood cells. Acta Endocrinol. 2019;15(1):9.
Okkay U, Okkay IF. Beneficial effects of linagliptin in a cell culture model of Parkinson’s disease. Eur Res J. 2022;8(2):242-6.
Marques C, Goncalves A, Pereira PMR, Almeida D, Martins B, Fontes-Ribeiro C, Reis F, Fernandes. The dipeptidyl peptidase 4 inhibitor sitagliptin improves oxidative stress and ameliorates glomerular lesions in a rat model of type 1 diabetes. Life Sci. 2019;234:116738.
Majeed SA, Hadi NR, Mudhafar AM Al, Al-Janabi HA. Sitagliptin ameliorates the progression of atherosclerosis via downregulation of the inflammatory and oxidative pathways. SAGE Open Med. 2013; 1:2050312113499912.
Alameen R, Bairam A, Al-Haddad M. Antioxidant and apoptotic activities of Sitagliptin against hepatocellular carcinoma: An in vitro study. F1000Res. 2023; 12:962.