LC-MS Chemical Profiling, In Silico Docking Studies to Unravel the Therapeutic Potential of Streptomyces hygroscopicus as a Source of Antimalarial Bioactive Compounds
Main Article Content
Abstract
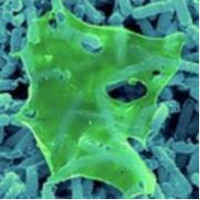
Malaria is a disease transmitted through the bite of female Anopheles mosquitoes carrying Plasmodium parasite. The resistance of the Plasmodium parasite against antimalarial drugs is a critical health concern necessitating the development of novel antimalarial treatments. Previous investigations reported that the crude extract of Streptomyces hygroscopicus Subsp. Hygroscopicus (S. hygroscopicus) possessed antimalarial properties, with in vitro assays confirming the ability to inhibit Plasmodium growth. Therefore, this research aimed to identify derivative compounds from S. hygroscopicus using Liquid Chromatography-Mass Spectrometry (LC-MS) and assess antimalarial activity by examining the binding site, pharmacokinetic profiles, and binding interactions through in silico analysis. In silico reverse molecular docking study was conducted with target proteins including Plasmodium falciparum malarial M1 aminopeptidase (PfA-M1), Plasmodium falciparum chloroquine resistance transporter (PfCRT), and falcipain-2 protease obtained from Protein Data Bank (PDB) and active compound ligands retrieved from PubChem. In addition, the analysis of pharmacokinetic profiles and bond interactions was performed using the SwissADME web tool and LigPlot software, respectively. The LC-MS analysis results showed that four compounds including dibenzyl amine, sedanolide, levalbuterol, and dibutyl phthalate with high retention times met the drug similarity criteria and had binding affinity values comparable to control ligands of the respective target proteins. The four compounds may have antimalarial activity due to the formation of hydrogen and hydrophobic bonds identical to those found between the target proteins and control ligands. Specifically, dibenzyl amine expressed the highest binding affinity across all target proteins, suggesting it as a potential antimalarial candidate.
Downloads
Article Details
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
How to Cite
References
Nchinda TC. Malaria: a reemerging disease in Africa. Emerg Infect Dis. 1998;4(3):398-403. DOI: https://doi.org/10.3201/eid0403.980313
Rollando R, Maulada F, Afthoni MH, Monica E, Yuniati Y, Nugraha AT. Screening Carica papaya compounds as an antimalarial agent: In silico study. Trop J Nat Prod Res. 2023;7(5):2895-2903. DOI: https://doi.org/10.26538/tjnpr/v7i5.9
Paengsri W, Promsawan N, Baramee A. Synthesis and evaluation of 2-hydroxy-1, 4-naphthoquinone derivatives as potent antimalarial agents. Chem Pharm B. 2021;69(3):253-7. DOI: https://doi.org/10.1248/cpb.c20-00770
WHO. World malaria report 2020: 20 years of global progress and challenges. 2020: xiv-xv
Ministry of Health of the Republic of Indonesia. Malaria Annual Report 2022:18.
Fola AA, Feleke SM, Mohammed H, Brhane BG, Hennelly CM, Assefa A, Crudal RM, Reichert E, Juliano JJ, Cunningham J, Mamo H, Solomon H,
Tasew G, Petros B, Parr JB, Bailey JA. Plasmodium falciparum resistant to artemisinin and diagnostics have emerged in Ethiopia. Nat Microbiol. 2023;8(10):1911-1919. DOI: https://doi.org/10.1038/s41564-023-01461-4
Fitri LE, Pawestri AR, Winaris N, Endharti AT, Khotimah ARH, Abidah HY, Huwae JTR. Antimalarial drug resistance: A brief history of its spread in
Indonesia. Drug Des Devel Ther. 2023;17:1995–201 DOI: https://doi.org/10.1016/0222-0776(96)89510-1
Nugraha RY, Faratisha IF, Mardhiyyah K, Ariel DG, Putri FF, Winarsih S. Nafisatuzzamrudah, Sardjono TW, Fitri LE. Antimalarial properties of isoquinoline derivative from Streptomyces hygroscopicus subsp. Hygroscopicus: an in silico approach. BioMed Res Inter. 2020; Article ID 6135696. DOI: https://doi.org/10.1155/2020/6135696
Ferreira LG, Dos Santos RN, Oliva G, Andricopulo AD. Molecular docking and structure-based drug design strategies. Mol. 2015;20(7):13384-421. DOI: https://doi.org/10.3390/molecules200713384
Cahyono AW, Fitri LE, Nafisatuzzamrudah, Nugraha RY, Aulia R, Febriliani F, Ariel DG, Mardhiyyah K, Winarsih S, Suciati, Japany D, Endang E,
Waluyo D, Non-Toxic fractions of Streptomyces hygroscopicus Subsp. Hygroscopicus metabolite suppressed the growth of Plasmodium falciparum in vitro possibly through L-malate: Quinone Oxidoreductase (PfMQO) mitochondrial enzyme inhibition. Sys Rev Pharm. 2020;11(10):524-31.
Fitri LE, Putri AM, Erwan NE, Putri FF, Nugraha RY, SardjonoTW, Mardhiyyah K, Ariel DG, Faratisha IF, Suciati, Ihsan BR, Winarsih S, Antimalarial properties of Streptomyces hygroscopicus subsp hygroscopicus secondary metabolite active fractions: in silico and in vivo analysis. Inter J Pharm Res. 2021;13(1):2553-67.
Wettersten HI, Ganti S, Weiss RH. Metabolomic profiling of tumor-bearing mice. In Met in Enz. Acad Press. 2014;543:275-296. DOI: https://doi.org/10.1016/B978-0-12-801329-8.00014-3
Egan TJ, Kuter D. Dual-functioning antimalarials that inhibit the chloroquine-resistance transporter. Fut Micro. 2013;8(4):475-89. DOI: https://doi.org/10.2217/fmb.13.18
Woods JA, Jewell C, O'Brien NM. Sedanolide, a natural phthalide from celery seed oil: effect on hydrogen peroxide and tert-butyl hydroperoxide-induced toxicity in HepG2 and CaCo-2 human cell lines. In Vit & Mol Tox: J Bas App Res. 2001;14(3):233-40. DOI: https://doi.org/10.1089/109793301753407984
Quintanilla LR, Mata CB, Vargas VJ, Bazaldúa RA, Ángeles HI, Garza GN, Hernandez GM, Antiprotozoal activity against Entamoeba histolytica of plants used in northeast Mexican traditional medicine. Bioactive compounds from Lippia graveolens and Ruta chalepensis. Mol. 2014; 19(12):21044-65. DOI: https://doi.org/10.3390/molecules191221044
Husain DR, Wardhani R. Antibacterial activity of endosymbiotic bacterial compound from Pheretima sp. earthworms inhibit the growth of Salmonella Typhi and Staphylococcus aureus: in vitro and in silico approach. Iranian J. Micro. 2021;13(4):537. DOI: https://doi.org/10.18502/ijm.v13i4.6981
Flydal MI, Kråkenes TA, Tai MD, Tran MP, Teigen K, Martinez A. Levalbuterol lowers the feedback inhibition by dopamine and delays misfolding and aggregation in tyrosine hydroxylase. Biochimie. 2021;183:126-32. DOI: https://doi.org/10.1016/j.biochi.2020.12.002
Jat KR, Khairwa A. Levalbuterol versus albuterol for acute asthma: a systematic review and meta-analysis. Pulmo Phar Ther. 2013;26(2):239-48. DOI: https://doi.org/10.1016/j.pupt.2012.11.003
Wang K, Yang H, Tang L. Virtual development of COVID-19 drugs targeting Nsp16-Nsp10 complex. J. Stud Res. 2023; 12(2). DOI: https://doi.org/10.47611/jsrhs.v12i2.4368
Mahmud F, Lai NS, How SE, Gansau JA, Mustaffa KMF, Leow CH, Osman H, Sidek HM, Embi N, Lee PC. Bioactivities and mode of actions of dibutyl phthalates and nocardamine from Streptomyces sp. H11809. Mol. 2022; 27(7):2292. DOI: https://doi.org/10.3390/molecules27072292
Li Y, Meng Q, Yang M, Liu D, Hou X, Tang L, Wang X, Lyu Y, Chen X, Liu K, Yu AM. Current trends in drug metabolism and pharmacokinetics. Acta Pharm Sin B. 2019; 9(6):1113-44. DOI: https://doi.org/10.1016/j.apsb.2019.10.001
Chaira T, Subramani C, Barman TK. ADME, pharmacokinetic scaling, pharmacodynamic and prediction of human dose and regimen of novel antiviral drugs. Pharmaceutics. 2023;15(4):1212. DOI: https://doi.org/10.3390/pharmaceutics15041212
Lipinski CA. Drug-like properties and the causes of poor solubility and poor permeability. J. Pharm Tox Met. 2000; 44(1):235-49. DOI: https://doi.org/10.1016/S1056-8719(00)00107-6
Veber DF, Johnson SR, Cheng HY, Smith BR, Ward KW, Kopple KD. Molecular properties that influence the oral bioavailability of drug candidates. J. Med Chem. 2002; 45(12):2615-23. DOI: https://doi.org/10.1021/jm020017n
Duru CE, Duru IA, Ikpa CBC, Enenebeaku UE, Obiagwu IC, Igbomezie MC, Nnabuchi MA. In silico docking studies of bioactive compounds in Ocimum gratissimum essential oil against candidapepsin-1 enzyme from Candida albicans. Trop J Nat Prod Res. 2021;5(2):364-369. DOI: https://doi.org/10.26538/tjnpr/v5i2.26
Seo S, Choi J, Park S, Ahn J. Binding affinity prediction for protein–ligand complex using deep attention mechanism based on intermolecular interactions. BMC Bioinformatics 2021;22:542. DOI: https://doi.org/10.1186/s12859-021-04466-0
Davarcioglu B. The general characteristic of weak intermolecular interactions in liquids and crystals. Inter J. Mod Eng Res. 2011;1(2):443-54.
Patil R, Das S, Stanley A, Yadav L, Sudhakar A, Varma AK. Optimized hydrophobic interactions and hydrogen bonding at the target-ligand interface leads the pathways of drug-designing. PLoS One. 2010;16;5(8):e12029. DOI: https://doi.org/10.1371/journal.pone.0012029
Mansouri M, Daware K,Webb CT, McGowan S. Understanding the structure and function of Plasmodium aminopeptidases to facilitate drug discovery. Curr. Opin. Struct. Biol. 2023; 82:102693. DOI: https://doi.org/10.1016/j.sbi.2023.102693
Wicht KJ, Mok S and Fidock DA. Molecular mechanisms of drug resistance in Plasmodium falciparum malaria. Ann Rev Micro. 2020;74:431-454. DOI: https://doi.org/10.1146/annurev-micro-020518-115546
Kim J, Tan YZ, Wicht KJ, Erramilli SK, Dhingra SK, Okombo J, Vendome J, Hagenah, LM, Giacometti SI, Warren AL. and Nosol K. Structure and drug resistance of the Plasmodium falciparum transporter PfCRT. Nat. 2019;576(7786):315-320. DOI: https://doi.org/10.1038/s41586-019-1795-x
Machin JM., Kantsadi AL. and Vakonakis I. The complex of Plasmodium falciparum falcipain-2 protease with an (E)-chalcone-based inhibitor highlights a novel, small, molecule-binding site. Malar. J. 2019;18(1):388. DOI: https://doi.org/10.1186/s12936-019-3043-0